|
|
|
| OJHAS Vol. 22, Issue 2:
April-June 2023 |
|
Case
Report
A
Rare Case of Fungaemia Due to Kodamaea
ohmeri in a Neonate
Authors:
Asem Ali Ashraf,
Department of Microbiology, Nitte
(Deemed to be University), KS Hegde
Medical Academy (KSHEMA), Deralakatte,
Mangalore-575018, Karnataka, India,
Vimal Kumar Karnaker,
Department of Microbiology, Nitte
(Deemed to be University), KS Hegde
Medical Academy (KSHEMA), Deralakatte,
Mangalore-575018, Karnataka, India,
Sreelatha Shankaran Veetil,
Department of Oral Pathology, AB Shetty
Memorial Institute of Dental Sciences
(ABSMIDS), Nitte (Deemed to be
University), Mangaluru- 575018,
Karnataka, India,
Sharika Ramdas,
Department of Microbiology, Nitte
(Deemed to be University), KS Hegde
Medical Academy (KSHEMA), Deralakatte,
Mangalore-575018, Karnataka, India,
Sanjana Nair, Srinivas Institute
of Medical Sciences and Research Centre,
Mangalore, Karnataka, India,
Sudhir Rama Varma, Clinical
Assistant Professor, Department of
Clinical Sciences, College of Dentistry,
Ajman University, Ajman, UAE Center for
Medical and Bio-allied Health Sciences
Research, Ajman University, Ajman, UAE.
Address for
Correspondence
Dr. Vimal Kumar
Karnaker,
Department of Microbiology,
KS Hegde Medical Academy (KSHEMA),
Nitte (Deemed to be University),
Mangalore, Karnataka, India.
E-mail:
vimalkarnaker@nitte.edu.in.
Citation
Ashraf AA, Karnaker VK,
Sreelatha SV, Ramdas S, Nair S, Varma
SR. A Rare Case of Fungaemia Due to Kodamaea
ohmeri in a Neonate. Online J
Health Allied Scs.
2023;22(2):11. Available at URL:
https://www.ojhas.org/issue86/2023-2-11.html
Submitted:
April
21, 2023; Accepted: July 8, 2023;
Published: July 15, 2023
|
|
|
|
| |
|
Abstract:
Background: K. ohmeri is seen
predominantly in cutaneous, endocarditis,
fungemia and catheter-related bloodstream
infections. Neonates are predisposed to systemic
fungal infections due to prematurity,
immunocompromised state, invasive procedures,
intubation, prolonged stay on ventilator and
antibiotic usage in neonatal intensive care
unit. The prevalence of K. ohmeri in a
new born has seldom been reported. Case
Presentation: We present an unusual
case of K. ohmeri fungemia in a
full-term neonate. A term male baby born to a
25-year-old primigravida mother at 39 weeks of
gestation age with birth weight of 2.5kgs via
normal vaginal delivery, with episodes of
hypoglycemia and multiple seizures was referred
to our institution for further medical
management. Sepsis screen showed elevated C
Reactive protein levels. Blood samples were sent
for microbial analysis. Culture yielded high
growth of white dry colonies which was
identified as K. ohmeri by VITEK 2
Compact System, and, matrix-assisted laser
desorption/ionization - time of flight based
automated bacterial identification system. Gram
stain of the positive blood culture sample had
shown numerous gram-positive oval-budding yeast
like cells. Anti-fungal susceptibility patterns
were evaluated and the child was put on
fluconazole. Conclusion: Clinical
antifungal treatment strategy for K. ohmeri
should be adjusted promptly according to
the susceptibility reports of the clinical
isolates rather than empirical drug use.
Key
Words: K. ohmeri,
endocarditis, fungemia, neonatal
|
|
Background
Kodamaea
ohmeri, a fungal micro-organism which
belongs to the Ascomycetae class and the
Saccharomycetaceae family, is the teleomorphic
form of Candida guilliermondii [1]. The
genus Kodamaea includes five species (K.
anthrophila, K. kakaduensis, K. laetipori, K.
nitidulidarum and K. ohmeri); K.
ohmeri being the only species that can grow
under 370C and infect humans [2]. It is
believed that K. ohmeri, formerly
considered as a contaminant, was first isolated
from a patient’s blood in 1998, and some decades
later, it has become an emerging human pathogen
that has witnessed a rise in severe infections as
well as high mortality rates, especially in
immunocompromised patients. Human infections due
to K. ohmeri have been reported
worldwide, predominantly cutaneous infection,
endocarditis, fungemia and catheter-related
bloodstream infections [3]. Neonates are
predisposed to systemic fungal infections due to
prematurity, immunocompromised state, invasive
procedures, intubation, prolonged stay on
ventilator and antibiotic usage in neonatal
intensive care unit (NICU). Not many cases have
been published of new-born fungemia with K.
ohmeri worldwide, including in India [4].
We present an unusual case of K. ohmeri
fungemia in a full-term neonate.
Case Presentation
A term male baby
born to a 25-year-old primigravida mother at 39
weeks of gestation age with birth weight of 2.5kgs
via normal vaginal delivery, with episodes of
hypoglycaemia and multiple seizures was referred
to our institution for further medical management.
At the time of presentation, head to toe
examination was normal and systemic examination
was within normal limits. The child had
hypoglycaemia and first episode of seizure at 30
hours of life following which IV fluids with
glucose infusion rate (GIR) of 6mg/kg/min were
initiated. However, at 40 hours of life, child was
lethargic with general random blood sugar (GRBS)
of 40mg/dl. Therefore, GIR of IV fluids had been
increased to 8mg/kg/min. Repeat GRBS was still
found to be low, as a consequence of which, IV
fluids were further continued at GIR of
10mg/kg/min. At 54 hours of life, the child had 2
episodes of seizures for which IV Levetiracetam
was initiated and maintenance dose Levetiracetam
was made oral by day 6. Lumbar puncture was done
to rule out meningitis. CSF (Cerebrospinal fluid)
analysis was within normal limits. Neurosonogram
done was within normal limits. GRBS was monitored
every four hours. No further episodes of
hypoglycaemia were noted. The child was euglycemic
for next 48 hours. IV fluids were tapered and
stopped by Day 7 of life. The child was initiated
on feeds by day 3 of life.
Sepsis screening
showed elevated CRP (C Reactive protein) levels
for which the child was initiated on Cefotaxime
(Meningitis Dose) along with IV Amikacin. Blood
samples were sent for further microbiological
analysis. Culture yielded high growth of white dry
colonies on 5% sheep blood agar. Gram stain of the
positive blood culture sample had shown numerous
gram-positive oval-budding yeast like cells.
Samples were streaked onto Sabouraud Dextrose Agar
(SDA). Dry and white colonies were isolated
following incubation at 30°C for 48 hours. These
dry and white growths were sub-cultured onto
CHROMagar Candida agar (Himedia, Mumbai, India)
and colonies were interpreted according to the
manufacturer’s instructions. White dry colonies
changing to light pink colonies were observed on
24-48 hours of incubation. On 48-72 hours of
incubation, light pink colour colonies changed to
blue colour colonies (Figure 1).
|

|
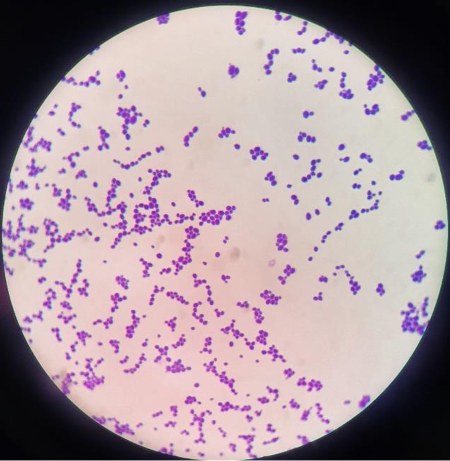
| Figure
1a: Gram stain of K.
ohmeri isolates (gram-positive
oval-budding yeast like cells) as observed
under oil immersion (100X). Total
Magnification: 1000x |
Figure
1b: Dry and white colonies were
isolated from Sabouraud Dextrose Agar
(SDA) following incubation at 30°C for 48
hours. |

|
| Figure 1c: K.
ohmeri isolates on CHROMagar
Candida agar. White dry colonies (Figure
1c1) changing to light pink colonies were
observed on 24-48 hours of incubation
(Figure 1c2). On 48-72 hours of
incubation, light pink colour colonies
changed to blue colour colonies (Figure
1c3). |
The isolate was
identified as K. ohmeri by VITEK 2
Compact System (BioMérieux, Marcy L’Etoile,
France) automatic identification system, as well
as, matrix-assisted laser desorption/ionization -
time of flight (MALDI -ToF) based automated
bacterial identification system (bioMerieux,
France). The anti-fungal susceptibility patterns
were evaluated (Table 1) and the
child was started on IV antifungal - Fluconazole.
After having received three days of IV
Fluconazole, the anti-fungal was made oral on day
9 of life. Repeat blood cultures were sent to rule
out contamination and the cultures had repeatedly
grown K. ohmeri. At day 9 of life, the
child had no episodes of vomiting, seizures,
icterus and was on direct breast feeding. A repeat
culture of blood sample showed no growth of K.
ohmeri. Clinical parameters were all
within normal limits and the neonate was being
discharged in a healthy clinical status. On
subsequent follow-up to the hospital for
evaluation, the neonate had no further episodes of
seizures or hypoglycaemia.
|
Table 1: The anti-fungal
susceptibility patterns
|
|
Antifungal
|
MIC*
|
Interpretation
|
|
Flucytosine
|
≤1
|
Sensitive
|
|
Fluconazole
|
2
|
Sensitive
|
|
Voriconazole
|
≤0.12
|
Sensitive
|
|
Amphotericin B
|
0.5
|
Sensitive
|
|
Caspofungin
|
0.25
|
Sensitive
|
|
Micafungin
|
0.12
|
Sensitive
|
|
* MIC- Minimal Inhibitory
concentration
|
Discussion and Conclusions
K. ohmeri
was first reported as a clinical isolate in 1984
from a pleural fluid sample; however, the isolate
was considered a contaminant at that time. In the
same year, K. ohmeri was isolated from a
blood sample of a 48-year-old diabetic patient
with immunosuppression in view of renal
transplantation, who subsequently died from the
infection. Since then, more invasive infections
with this yeast have been reported globally and
considering it a true clinical pathogen, K.
ohmeri have caused several life-threatening
infections mainly in immunocompromised
individuals. Comorbidities (like malignancy,
diabetes, and rheumatism) and central venous
catheter implantation are the commonest
predisposing factors. Other factors that can also
be a potential risk factor for K. ohmeri
infections include invasive procedures which can
breech the skin mucosal barrier, including
surgery, catheterization, and dialysis [2, 3, 4].
In our case report,
we describe an uncommon case of fungaemia in a
child caused by K. ohmeri, with no known
co morbidities and no risk factors. It can be
concluded that infections by K. ohmeri
occur in a broad range of patient categories,
including neonates and children [5]. Albeit common
amongst immune-compromised patients, there are
risk factors also reported in children, which
include: prematurity, low birth weight, prolonged
ICU stay, use of medical devices, prosthetic
valves, usage of broad-spectrum antibiotics, total
parenteral nutrition, immunosuppression
(leukemias, lymphomas) and neutropenia. To date,
there is only one case reported of infection in a
previously healthy child with no predisposing
conditions except for encephalitis [3,6].
As a rare fungal
pathogen isolated in the clinical setting, the
identification of K. ohmeri was most
commonly mistaken for Candida albicans,
Candida glabrata, and Candida
tropicalis, based on the colony morphology.
In most clinical microbiology laboratory, the
CHROMagar Candida chromogenic growth medium is a
helpful culture medium for identification of
Candida species based on the varying coloured
colonies. K. ohmeri can grow yeast-like
colonies on CHROMagar, the colour of which change
from pink/lilac to blue in 2–3 days. Since the
colour change takes time and often requires the
need for continuous observation, the
misidentification rate of CHROMagar in identifying
K. ohmeri can be quite high (up to 100%)
if only one single observation is performed in
routine laboratory work. [1].
VITEK 2 ID-YST
system allows for more accurate identification,
even though some cases of misidentification with C.
haemulonii have been illustrated [7]. Rapid
identification of K. ohmeri in clinical
laboratories have been successfully done in
several cases since the development and use of
MALDI-TOF MS has enabled rapid identification of Candida
species in clinical laboratories [1].The accuracy
of MALDI-TOF for K. ohmeri
identification was comparable to that of PCR,
hence, DNA sequencing of ITS 1 and 2 or MALDI-TOF
apparently seem to be the gold standard techniques
for the identification of K.ohmeri, even
though their use is limited due to cost and
availability in everyday practice [7].
Treatment of K.
ohmeri infection includes removal of the
risk factors (such as central venous catheter
implantation and mechanical ventilation) and
administration of appropriate antifungal agents.
Various antifungal regimens were used in the
treatment of K. ohmeri infection [1]. No
intrinsic resistance of K. ohmeri to
antifungals has been reported to date. There have
been several reports of fluconazole resistance,
some reports of echinocandin resistance and only
one report of an isolate with high MIC's to
amphotericin B [3]. Therefore, the clinical
antifungal treatment strategy should be adjusted
promptly according to the susceptibility reports
of the clinical isolates rather than empirical
drug use [1].
Abbreviations
NICU: Neonatal
intensive care unit; GIC: Glucose infusion rate;
GRBS: General random blood sugar; CRP: C Reactive
protein; CSF: Cerebrospinal fluid analysis; MALDI
-ToF: Matrix-assisted laser desorption/ionization
- time of flight; SDA: Sabouraud Dextrose Agar;
MIC: Minimal Inhibitory concentration
References
- Diallo K, Lefevre B, Cadelis G, Gallois JC,
Gandon F, Nicolas M, et al. A case report of
fungemia due to Kodamaea ohmeri. BMC
Infect Dis. 2019;19(1):570. doi:
10.1186/s12879-019-4208-8.
- Vivas R, Beltran C, Munera MI, Trujillo M,
Restrepo A, Garcés C. Fungemia due to Kodamaea
ohmeri in a young infant and review of
the literature. Med Mycol Case Rep.
2016; 20: 13:5-8. doi:
10.1016/j.mmcr.2016.06.001
- Zhou M, Li Y, Kudinha T, Xu Y and Liu Z.
Kodamaea ohmeri as an Emerging Human Pathogen: A
Review and Update. Front. Microbiol. 2021;
12:736582. doi: 10.3389/fmicb.2021.736582
- Borade A, Kapdi M, Suryavanshi K. Kodamaea
Ohmeri - An Emerging Fungal Pathogen in
Neonatal Intensive Care Unit. Pediatr On
call J. 2014;11: 114-116.doi:
10.7199/ped.oncall.2014.66
- De Barros JD, Do Nascimento SM, De Araújo FJ,
BrazRde F, Andrade VS, Theelen B, et al. Kodamaea
(Pichia) ohmeri fungemia in a
pediatric patient admitted in a public hospital.
Med Mycol. 2009;47(7):775-9. doi:
10.3109/13693780902980467.
- Otag F, Kuyucu N, Erturan Z, Sen S, Emekdas G,
Sugita T. An outbreak of Pichia ohmeri
infection in the Paediatric Intensive Care Unit:
Case Reports and review of the literature. Mycoses.
2005;48(4):265–9. doi:
10.1111/j.1439-0507.2005.01126.x
- Ioannou P, Papakitsou I. Kodamaea ohmeri
infections in humans: A systematic review. Mycoses.
2020;63(7):636-643. doi: 10.1111/myc.13094
|
|



















