|
Introduction
Superficial
spreading squamous cell carcinoma (SCC) of the
cervix is a rare phenomenon. The spread usually
occurs by direct local extension, lymphatic
embolization and by hematogenous dissemination.
Direct extension to the lower uterine segment
and/or endometrial cavity occurs in about 10% to
30% of patients [1]. However, the upward
superficial contigous spread of endometrium and
fallopian tube is much rare with fewer than 20
cases reported in literature.
Case Report
A 65-year-old post
menopausal woman presented with foul smelling,
white discharge per vagina since 1 month. The
clinical diagnosis was cervical stenosis with
pyometra. Cervical dilation was done and biopsies
were obtained from cervix and endometrium.
Microscopically, both cervix and endometrium
showed severe squamous dysplasia. The patient
subsequently underwent total hysterectomy with
bilateral salpingo-oophorectomy. Grossly, the
uterus with cervix measured 8 x 6 x 3 cm. On cut
section, the endometrial cavity was dilated and
exuded 15 ml of thick brown colour fluid. (Fig. 1)
The cervix appeared unremarkable and the left
fallopian tube on cutting exuded purulent material
with dilated lumen.
Microscopically, the
cervix showed squamous cell carcinoma in situ with
moderate inflammation in the stroma. There was
upward surface extension into isthmus with
complete replacement of endometrial lining and
left fallopian tube epithelium by carcinoma in
situ. (Fig 2,3,4). The spread was contiguous and
there was no stromal invasion in any of these
sites. Immunohistochemistry with p16 showed
diffuse, intense positivity of dysplastic
stratified squamous epithelium in all the sites.

|

|
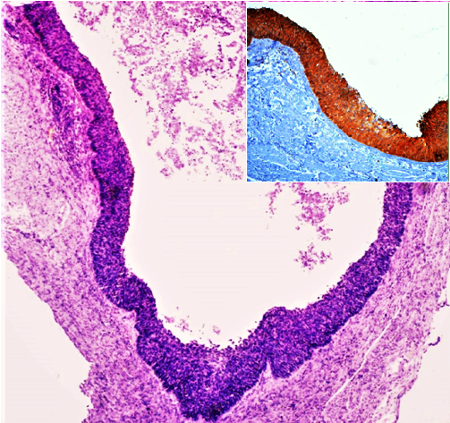
| Fig
1: Specimen of uterus with dilated
endometrial cavity |
Fig
2: Cervix showing severe dysplasia
(H&E x100, Inset- P16 overexpression
IHC, x100) |

|
|
| Fig
3: Endometrium showing squamous cell
carcinoma in situ (H&E x100, Inset-
P16 overexpression IHC, x40) |
Fig
4: Left side Fallopian tube showing
carcinoma in situ (H&E x100, P16
overexpression IHC, x40) |
Discussion
Cervical cancer
continues to be a common malignancy affecting
middle-aged women, particularly in less-resourced
countries [2]. The primary routes of spread of
cervical carcinoma are direct local extension and
lymphatic embolization. The hematogenous
dissemination usually occurs with more advanced
disease or unusual cell types. Direct extension to
the lower uterine segment and/or endometrial
cavity occurs in about 10% to 30% of patients [1].
Cervical SCC that
spreads superficially to the inner surface of the
uterus replacing the endometrium with carcinoma
cells is called superficial spreading SCC, which
is a very rare phenomenon [3].
Baggish &
Woodruff did a comprehensive literature search and
presented a classification of histogenesis of
squamous epithelium in the endometrium. They noted
that the presence of squamous epithelium in
endometrium occur in conditions varying from
physiological as in endometrial shedding, non
neoplastic conditions like foreign bodies, chronic
inflammation etc, and underlying benign and
malignant neoplasms. They emphasized on the
careful study of each case in order to eliminate
the possibility of extension of squamous cell
carcinoma of cervix. They cited a case of cancer
cervix with extension into endometrial surface and
fallopian tube. They have also mentioned about the
occurrence of a similar case in their laboratory.
Since then, many cases of squamous cell carcinoma
extending into the endometrium have been reported.
Some authors are of the opinion that they were two
cancers occurring simultaneously and were
coincidental, while others attributed it to post
radiotherapy treatment in diagnosed cases of
cancer cervix [4].
Superficial
spreading SCC of the cervix is a rare phenomenon,
with few cases reported in literature. The search
of English literature revealed contiguous spread
of SCC cervix into endometrium and fallopian tubes
in nineteen cases, out of which 8 cases showed
involvement of ovaries. One case among them also
showed omental deposits. (Table 1)
|
Table 1: Superficial spreading
carcinoma of cervix with proximal
extension into upper genital tract
|
|
Authors
|
Age (yrs)
|
Clinical features
|
Cervix
|
Uterus
|
Fallopian tube
|
Ovaries
|
Others
|
|
1.
|
Langley & Woodcock 4,7
(1954)
|
64
|
Not recorded
|
Invasive SCC
|
In situ and invasive
|
Left –isthmus and ampullary portion- in
situ
|
|
Post surgery death
|
|
2
|
Baggish4 (1967)
|
?
|
Not recorded
|
No residual cancer
|
Involved-extent not known
|
Surface involvement
|
|
RT 21/2 years ago
|
|
3
|
Willis7 (1967)
|
48
|
Post radiation Pyometra
|
Invasive SCC
|
Involved- extent not known
|
Bilateral
|
Bilateral
|
|
|
4
|
Hall Grimsson7 (1967)
|
54
|
Pyometra
|
Ca in situ
|
Involved- extent not known
|
Bilateral
|
|
|
|
5
|
Weill7 (1968)
|
69
|
Pyometra
|
Ca in situ
|
Involved- extent not known
|
Bilateral
|
|
|
|
6
|
Quizilibash6
(1975)
|
63
|
Not recorded
|
Invasive SCC
|
Involved-in situ
|
Bilateral-in-situ
|
|
|
|
7
|
Kanbour 7 (1978)
|
66
|
Pyometra
|
Invasive SCC
|
Is-situ with microinvasion
|
Fallopian tube-in-situ
|
|
|
|
8
|
Voet RL13 (1979)
|
68
|
Pyometra
|
Ca in situ
|
Involved
|
Right fallopian tube
|
|
|
|
9
|
Punnonen R8 (1979)
|
64
|
Abnormal PAP smear- routine
|
Invasive SCC
|
In-situ, in glands
|
Right fallopian tube-in situ
|
|
|
|
10
|
Sandhyamani S15 (1983)
|
-
|
-
|
In-situ
|
In-situ
|
In-situ
|
|
Vagina
|
|
11
|
Motoyama T9 (1988)
|
59
|
Vaginal bleeding
|
Invasive SCC
|
Endometrium and underlying stromal
sarcoma
|
Left fallopian tube, in-situ
|
Left ovarian cyst lining
|
Vagina, Vulva involved
|
|
12
|
Pins MR11 (1997)
|
55
|
Pyometra
|
Ca in situ
|
In situ
|
Bilateral-invasive
|
Bilateral –surface and parenchymal
|
|
|
13
|
Kushima13 (2001)
|
68
|
Vaginal discharge
|
Ca in situ
|
CIS with Microinvasion
|
Left- invasive
|
Left-invasive
|
|
|
14
|
59
|
Vaginal discharge
|
Deeply invasive
|
Microinvasive
|
Left- in situ
|
Left ovary- invasive
|
|
|
15
|
Agashe S R16 (2007)
|
|
-
|
Ca in situ
|
Superficial extension
|
Bilateral
|
Bilateral
|
|
|
16
|
Gungor T3 (2011)
|
53
|
Postmenopausal Bleeding PV
|
Micro invasive SCC
|
Invasive
|
Bilateral
|
Bilateral
|
|
|
17
|
Chao A 3 (2013)
|
60
|
Pyometra, abdominal distension and
abdominal mass
|
Ca in situ
|
Invasive
|
Bilateral
|
|
Died 2 days after surgery
|
|
18
|
Nakajima J10 (2019)
|
67
|
Pain abdomen
|
Ca in situ
|
Ca in situ
|
Bilateral –in situ
|
Bilateral -superficial
|
Omentum involved
|
|
19
|
Present case (2020)
|
65
|
Foul smelling discharge
|
Ca-in situ
|
Ca-in situ
|
Left fallopian tube, Ca- in situ
|
-
|
|
The main clinical
manifestations include vaginal bleeding, pyometra,
abdominal mass, lower abdominal pain, abnormal pap
smears, hematometra, and excessive genital
discharge. Our patient presented with foul
smelling vaginal discharge and pyometra. In any
postmenopausal woman with pyometra, if widespread
keratinization of endometrial surface is detected
in the curettage or biopsy, then careful
examination should be done to rule out an
underlying malignancy [3]. The pathology of
cervical neoplasia varied from SCC in situ,
invasive SCC, microinvasive SCC and the pattern of
spread in the endometrium, fallopian tubes and
ovaries were also in situ and invasive [5].
The diagnosis of
superficial spreading SCC of the uterine cervix
involving the endometrium requires careful
examination of the uterine body and the cervix to
rule out primary endometrial SCC. This is based on
the following strict pathological criteria
recommended by Fluhmann: (1) no evidence of a
coexisting endometrial adenocarcinoma or primary
cervical SCC (2) no connection between the
endometrial tumour and squamous epithelium of the
cervix; or (3) no connection between any existing
cervical in situ carcinoma and the independent
endometrial neoplasm. In the present case, we
demonstrated the continuity of the cervical lesion
to the endometrium and fallopian tube, conforming
Fluhmann criteria [3,6].
Intraepithelial
carcinoma of the vagina and endometrium are seen
in association with cervical cancer at a frequency
of 2.0% and 0.7% respectively [7]. The common
patterns of uterine corpus involvement by cervical
cancer are through deep myometrial penetration and
lymphatic dissemination. The association of
endometrial lesion in the presence of cervical
cancer is usually assumed to result from a
“horizontal spread” as postulated by Cullen and
Ferenczy et al where cervical neoplastic cells
mechanically displace and eventually replace the
benign glandular epithelium of the endometrium.
The second mechanism is a process in which the
normal cell transforms to malignant cell,
proliferates vertically (Field theory of
carcinogenesis), with occurrence of carcinoma
cervix and endometrium independently and
concurrently by the same cancer stimulating agent.
The superficial surface spread of in situ or
invasive squamous carcinoma of cervix over the
contiguous endometrial surface may be evident on
gross inspection as whitish patches, a condition
called "cake icing" or "Zuckerguss" carcinoma.
[5,6,7]. Histological continuity between cervical,
endometrial and fallopian tube lesion is often
demonstrated as in the present case. Qizilbash
proposed that the cervical stenosis and subsequent
pyometra could have a promoting effect for surface
propagation of cervical cancer. The mitotic
activity is an essential criterion for the
diagnosis of carcinoma in situ of the tube as
proposed by Pauerstein & Woodruff. [6,8].
The World Health
Organization (WHO) in its classification of tumors
of the cervix and Federation of International
Gynecologists & Obstetricians (FIGO) in cancer
staging have not described such an event. It may
be essential to include this phenomenon as
occasional cases of superficial spreading SCC are
reported with extension into bilateral fallopian
tubes, ovaries and even spread to lymphnodes and
omentum. However, the prognostic significance is
lacking with the available limited data. The study
of more cases are therefore needed to determine
management guidelines and prognosis [3,9,10].
Pins MR et al
investigated for the presence of HPV genome by PCR
analysis and noted its presence in a case of
cervical carcinoma in situ with spread to
endometrium, bilateral fallopian tubes with focal
invasion and bilateral ovarian surface and
parenchyma. This supported the contiguous spread
of tumor [11]. However, Kushima et al are of the
opinion that the presence of HPV16 throughout the
lesions does not necessarily support contiguous
spread but rather consistent with a field effect
by an infectious agent. They recommend genetic
analysis to establish the monoclonality of such
lesions. They described five cases of unusual
superficial spread of cervical SCC and performed
genetic analysis which suggested a single clonal
process with frequent loss of heterozygosity of
6p, 6q, 11p and 11q. Thus, they indicated that
these tumors originated from the cervix and
extended superficially to the upper genital tract.
We performed IHC with p16 and found the dysplastic
epithelium to be diffusely and strongly positive
in all the sites. We believe that dysplastic
features on histology along with p16 as a
surrogate marker for HPV would be of considerable
value in establishing the origin of the tumor. A
number of studies have demonstrated p16 to be a
useful, robust, specific and sensitive biomarker
marker for squamous and glandular epithelial
dysplasia in the uterine cervix and appears to
correlate with the degree of cervical neoplasia.
This was explained in two ways: the most possible
explanation for the composite of findings is that
a HPV associated squamous cell dysplasia
originated in the cervix and extended proximally
in a purely lepidic pattern with surface extension
or by colonizing a pre-existing ichthyosis uteri
[5,12,13]. Some authors have described SCC of
cervix with dysplastic epithelium in uterus as
ichthyosis uteri showing dysplastic changes [14].
A strong expression of CD138 has been demonstrated
in carcinoma cells that participate in superficial
spreading by regulating cell to cell interactions
while cells in the invasive focus lacking CD138
expression [5]. However, CD138 was not done in the
present case.
Total abdominal
hysterectomy with bilateral salpingo-oophorectomy
is the optimal therapy for superficial spreading
SCC, however, the available data are insufficient
to evaluate the role of additional radiotherapy or
chemotherapy [3,13].
Conclusion
Superficial
spreading squamous cell carcinoma in situ of
cervix with surface extension into endometrium and
fallopian tube is rare and very few cases are
reported. IHC with p16 may be used as a surrogate
marker to establish the histogenesis. More cases
are needed to understand the therapeutic and
prognostic implications.
References
- Gallup D. The Spread and Staging of Cervical
Cancer. Glob.libr. Women’s med, (ISSN:
1756-2228) 2008; DOI 10.3843/GLOWM.10231.
Available at https://www.glowm.com/section-view/heading/The%20Spread%20and%20Staging%20of%20Cervical%20Cancer/item/231
- Arbyn M, Weiderpass E, Bruni L, Sanjose S,
Saraiya M, Ferlay J. Estimates of incidence and
mortality of cervical cancer in 2018: a
worldwide analysis. The Lancet of Global
Health. 2020;8(2) DOI:
https://doi.org/10.101: 6/S2214-109X(19)30482-6
- Du Jing, Liao X. Case Report Superficial
spreading squamous cell carcinoma in situ of the
cervix involving the endometrium: a rare case
presentation and review of literature. Int J
Clin Exp Pathol 2019;12(11):4162-4166
- Baggish MS, Woodruff JD. The occurrence of
squamous epithelium in the endometrium. Obstet
Gynecol Surg 1967;22:69–115.
- Muthusamy RK, Mehta SS. Squamous cell
carcinoma in situ of the cervix with superficial
intraepithelial extension to the endometrium of
lower uterine segment: a rare presentation. Indian
J Med Paediatr Oncol 2017;38: 88-89.
- Qizilbash A, DePedrillo A. Endometrial and
tubal involvement by squamous carcinoma of the
cervix. Am J Clin Pathol 1975;64:
668–71.
- Kanbour AI, Stock RJ. Squamous cell carcinoma
in situ of the endometrium and fallopian tube as
superficial extension of invasive cervical
carcinoma. Cancer 1978;42:570–80.
- Punnonen R, Grönroos M and Vaajalahti P.
Squamous cell carcinoma in situ from the uterine
cervix to the distal end of the fallopian tube.
Acta Obstet Gynecol Scand 1979;58:
101-104.
- Motoyama T, Watanabe H. Squamous cell
carcinoma of the cervix with extensive
superficial spreading to almost whole genital
tract and associated with endometrial stromal
sarcoma. Acta Pathol Jpn
1988;38:1445–52.
- Nakajima T, Hatta H, Nishida T, Minamisaka T,
Miwa S, Terahata S, Imura J. Superficial spread
of cervical squamous cell carcinoma to the upper
genital tract and dissemination to the omentum.
Pathol Int 2019;69:119-121.
- Pins MR, Young RH, Crum CP, et al. Cervical
squamous cell carcinoma in situ with
intraepithelial extension to the upper genital
tract and invasion of tubes and ovaries: report
of a case with human papilloma virus analysis. Int
J Gynecol Pathol 1997;16:272–8.
- Lesnikova I, Lidang M, Hamilton-Dutoit S. et
al. p16 as a diagnostic marker of cervical
neoplasia: a tissue microarray study of 796
archival specimens. Diagn Pathol.
2009;4: 22.
https://doi.org/10.1186/1746-1596-4-22
- Kushima M, Fujii H, Murakami K, Ota H,
Matsumoto T, Motoyama T, Kiyokawa T, Ishikura H.
Simultaneous squamous cell carcinomas of the
uterine cervix and upper genital tract: loss of
heterozygosity analysis demonstrates clonal
neoplasms of cervical origin. Int J Gynecol
Pathol 2001;20:353-358.
|



















