|
Introduction
Ectopic
thyroid tissue (ETT) refers to thyroid follicular
tissue that is located outside of the thyroid bed,
which is a rare phenomena, primarily caused by
embryologic disorders and dysgenesis and has an
incidence of 1 case per 1,00,000 individuals. The
base of the tongue(~90%) is the most common
ectopic site and is followed by sublingual and
intratracheal region in the midline neck(1).
Ectopic thyroid tissue is occasionally encountered
within the lateral neck node resected from
patients with thyroid carcinomas which accounts
for only 1% - 3% of thyroid ectopies(2).
Distinguishing benign thyroid tissue and a nodal
metastasis can be challenging and has direct
impact on staging and treatment(3).
Case Report
A 64 year old male
presented with anterior neck swelling for the past
20 years. On examination a swelling of size 5 x 5
cm was present in the anterior aspect of neck,
firm in consistency and lower lobes were not
palpable. Fine needle aspiration cytology of
thyroid showed thyroid follicular cells with
overcrowding and many nuclei showing nuclear
grooving, suggestive of Bethesda category III-
Atypia of undetermined significance.
Patient underwent
total thyroidectomy with bilateral neck node
dissection. Gross examination showed an ill
defined infiltrating lesion of size 6 x 3.5 x 1.5
cm; 3.9 x 1.9 x 1.4 cm and 0.4 x 0.4 cm involving
right lobe, left lobe and isthmus respectively
with macroscopic extension into the adjacent strap
muscles. Histopathology revealed an infiltrating
tumor arranged in broad papillae with tumor cells
exhibiting moderate nuclear pleomorphism and
mitosis of <3 per mm2, with foci of
nuclear crowding, overlapping and infiltration
into strap muscles. Microscopic examination of
bilateral neck nodes showed an incidental finding
with foci of thyroid inclusion consisting of
normal appearing thyroid follicles in the
subcapsular region of the lymph node. They
exhibited no papillarity or nuclear atypism and no
psammoma bodies, with rest of the lymph nodes
showing reactive lymphoid hyperplasia. On
retrospective examination of lymph nodes, the cut
surface of both the lymph nodes were unremarkable.
Considering all these factors, a comprehensive
diagnosis of conventional papillary carcinoma
thyroid, involving both lobes of thyroid and
isthmus with extrathyroidal extension into strap
muscles and benign thyroid inclusions of bilateral
neck nodes was made.
|
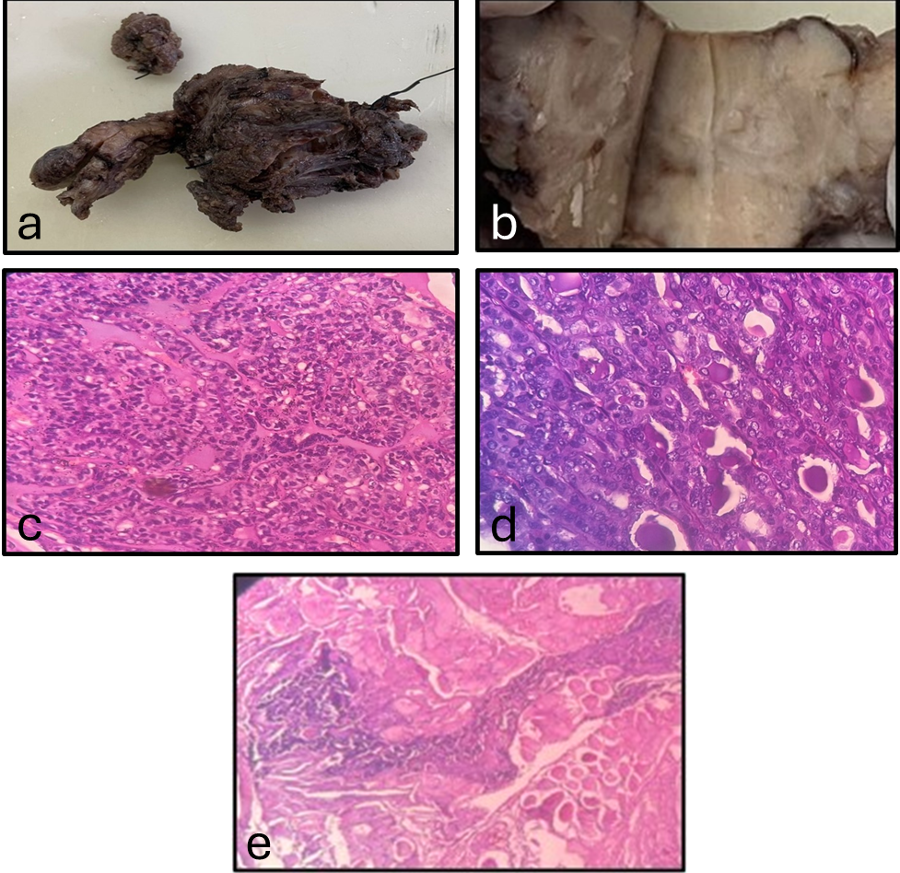
Figure
1: Right and left lobe of thyroid with
isthmus (a); cut surface showing
ill-defined grey-white infiltrating lesion
(b); tumor cells arranged in papillae
(c,d); tumor infiltrating into the strap
muscles (e)
|
|
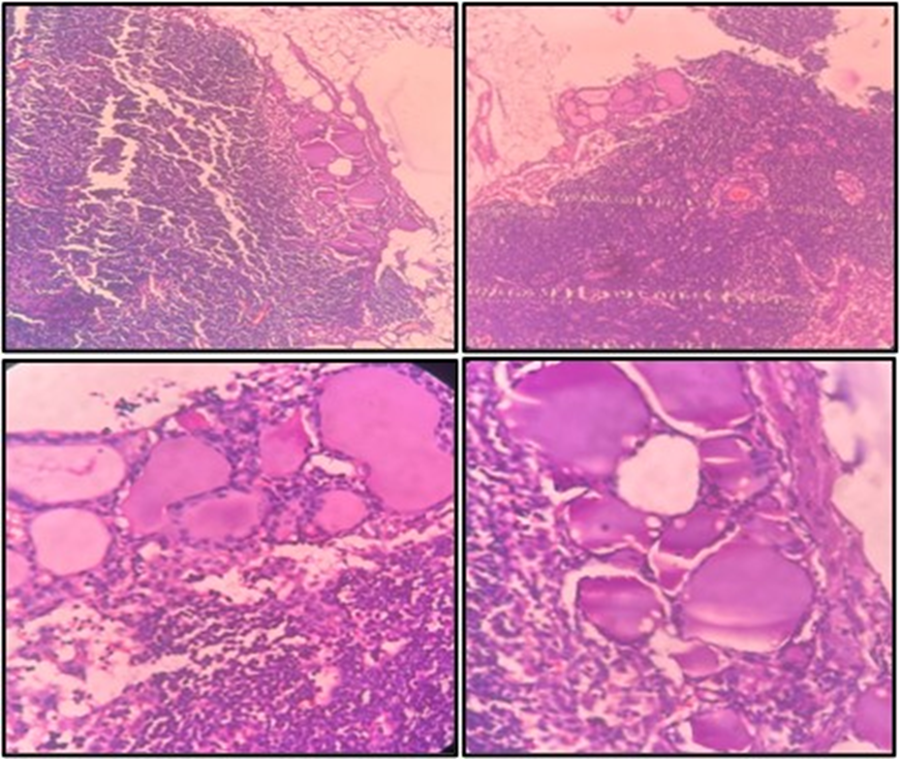
| Figure 2: Bilateral neck
nodes- showing well-formed thyroid
inclusions containing clusters of normal
appearing thyroid follicles lined by
flattened to cuboidal epithelium filled
with colloid. No papillary/nuclear
features seen. |
Discussion
Benign thyroid
inclusions occur in various anatomical site and
clinical conditions and includes both benign and
malignant differential diagnosis. During embryonic
development, migration of thyroid tissue can
result in ectopic depositions in different parts
of the body. ETTs have been reported in heart,
lung, mediastinum, ovaries, adrenals, duodenum,
pancreas, intestine and various locations in the
neck and throat(4). There have only been 17
reports of benign thyroid tissue in neck lymph
nodes in the previous 20 years, making it an
uncommon condition(5,6). It has been proposed that
abnormalities that result in ejection of thyroid
tissue from the gland, and migration via the
lymphatic system during embryogenesis may result
in ETT in lymph nodes(5).
Thyroid inclusions
in neck lymph nodes need to be differentiated from
several other conditions. These include (a)
Displaced masses of thyroid tissue, in the neck
outside of lymph nodes, for which a connection to
the thyroid gland is often demonstrated; (b)
Lateral aberrant thyroid tumors, which are thought
to be metastatic papillary carcinomas; (c) struma
lymphomatosa, characterized by hyperplastic
lymphoid tissue with germinal centers surrounding
the group of thyroid follicles within the thyroid
gland and (d) thyroid tissue can be implanted in
the soft tissue of the neck following a
thyroidectomy, even at a considerable distance
from the site of the incision(7).
Distinguishing nodal
metastasis of primary thyroid cancer from ETT in
neck lymph nodes can be challenging. This is due
to the fact that all thyroid tissue found in lymph
nodes are often considered as malignant(3,8).
Histologic criteria has been proposed to
distinguish benign thyroid inclusions from
malignant in lymph nodes(5,6). This comprises the
extent and morphology of thyroid follicles,
absence of psammoma bodies, absence of
desmoplastic stroma, immunohistochemistry and
molecular profiling(3). It is possible to
differentiate benign thyroid tissue and thyroid
carcinoma in lymph node; if the thyroid tissue
satisfies the criteria in Table 1.(5,9)
|
Table 1: Suggested criteria for
differentiation of Benign thyroid tissue
and metastasis in lymph node
|
|
Features
|
Benign thyroid tissue
|
Nodal metastasis
|
|
Evidence of primary tumor
|
Absent
|
Thyroid carcinoma –most commonly
papillary
|
|
Cervical lymph node involvement in
relation to jugular vein
|
Medial
|
Mainly inferior and lateral
|
|
Extent
|
Single focus of few follicles in
subcapsular or intracapsular region within
the lymph node.
|
From few follicles to total replacement
of lymph node.
|
|
Number of lymph node involvement
|
One, rarely 2 lymph nodes.
|
Multiple nodes involved
|
| Size of the lymph node |
Microscopic size |
Macroscopicaly enlarged |
Microscopic
features
|
| Architectural pattern |
Normal-appearing thyroid follicles-
regular in size and shape containing
abundant colloid. |
Papillary / solid pattern. |
| Nuclear features |
No features of papillary thyroid
carcinoma(PTC) |
Nuclear enlargement, crowding, inclusions,
optical clearing etc. |
| Psammoma bodies |
Absent |
Present |
|
Stromal reaction
|
Absent
|
Present
|
|
IHC
|
TTF+, Tg+, CK19-, Gal3-, HBME1-
|
CK19+, Gal3+, HBME1+
|
|
Molecular testing
|
No aberrations
|
BRAF+, RET/PTC+, RAS+
|
|
Clonality
|
Polyclonal
|
Monoclonal
|
According to autopsy
or neck dissection, the probability of benign
thyroid inclusions or psammoma bodies in patients
who have had cervical lymphadenectomy is about
0.8% and 0.6 to 0.5% in head and neck lymph nodes
respectively(6,10). Thus the discrimination
requires caution because benign intranodal thyroid
tissue may falsely show up as metastasis of occult
thyroid carcinoma in neck lymph nodes. In the
present case, bilateral neck node dissection done
for suspicion of thyroid carcinoma showed clusters
of thyroid follicles lined by flattened to
cuboidal epithelium containing abundant colloid
located within subcapsular region of the lymph
node, histopathologicaly confirmed as benign
thyroid inclusions considering the macroscopic,
cytologic and nuclear features. Since the
histopathological examination was imperative of
benign appearing thyroid glandular tissue with
colloid and flattened epithelial lining,
confirmation using immunohistochemistry was not
done.
To conclude, thyroid
inclusions within lateral neck nodes is a rare
benign entity and does not always indicate nodal
metastasis of thyroid malignancy. Distinguishing
benign thyroid tissue from malignant and other
non-neoplastic conditions is essential as it has
direct impact on staging, treatment and further
management.
References
- Zhang Y, Zheng X, Wang X et al. Ectopic
thyroid tissue in the lateral lymph nodes: A
rare case and literature review, 05 September
2023, PrePrint (Version 1) available at Research
Square [https://doi.org/10.21203/rs.3.rs-3292286/v1]
- Prado H, Prado A, Castillo B. Lateral ectopic
thyroid: a case diagnosed preoperatively. Ear
Nose Throat J. 2012 Apr;91(4):E14-8. doi:
10.1177/014556131209100417.
- Gijsen AF, De Bruijn KMJ, Mastboom W. Thyroid
tissue in cervical lymph nodes, not always
malignant. Clin Case Rep. 2022 Sep
6;10(9):e6261. doi: 10.1002/ccr3.6261.
- Noussios G, Anagnostis P, Goulis DG, Lappas D,
Natsis K. Ectopic thyroid tissue: anatomical,
clinical, and surgical implications of a rare
entity. Eur J Endocrinol. 2011
Sep;165(3):375-82. doi: 10.1530/EJE-11-0461.
- Triantafyllou A, Williams MD, Angelos P et al.
Incidental findings of thyroid tissue in
cervical lymph nodes: old controversy not yet
resolved? Eur Arch Otorhinolaryngol. 2016
Oct;273(10):2867-75. doi:
10.1007/s00405-015-3786-3.
- Ansari-Lari MA, Westra WH. The prevalence and
significance of clinically unsuspected neoplasms
in cervical lymph nodes. Head Neck. 2003
Oct;25(10):841-7. doi: 10.1002/hed.10304.
- Roth LM. Inclusions of Non-Neoplastic Thyroid
Tissue Within Cervical Lymph Nodes. Cancer.
1965 Jan;18:105-11.
- Butler JJ, Tulinius H, Ibanez ML, Ballantyne
AJ, Clark RL. Significance of thyroid tissue in
lymph nodes associated with carcinoma of the
head, neck or lung. Cancer. 1967
Jan;20(1):103-12.
- Meyer JS, Steinberg LS. Microscopically benign
thyroid follicles in cervical lymph nodes.
Serial section study of lymph node inclusions
and entire thyroid gland in 5 cases. Cancer.
1969 Aug;24(2):302-11.
- Lee YJ, Kim DW, Park HK, Ha TK, Kim DH, Jung
SJ, Bae SK. Benign intranodal thyroid tissue
mimicking nodal metastasis in a patient with
papillary thyroid carcinoma: A case report. Head
Neck. 2015 Sep;37(9):E106-8. doi:
10.1002/hed.23886.
|



















