|
Introduction
A
diaphragmatic hernia (DH) is defined as a
protrusion of abdominal viscera into the thoracic
cavity through a defect within the diaphragm. Most
commonly the disorder is congenital in nature,
arising due to the failure of complete
diaphragmatic fusion during embryologic
development. The less common acquired variant is
secondary to blunt or penetrating trauma to the
abdomen / thorax or iatrogenic causes [1, 2], and
generally termed as posttraumatic diaphragmatic
hernias (PTDHs). The presentation may be acute
with haemodynamic and respiratory instability or
else, they may go undiagnosed at the initial
trauma at all and manifest months or years later
as a diaphragmatic hernia [3]. They can present a
diagnostic and therapeutic challenge and have an
overall mortality rate of up to 31% [4].
In this retrospective analysis, we describe our
experience with patients who reported to the
general surgical unit of a medical college in the
Kashmir Valley with delayed presentations of PTDH.
Materials and Methods
A retrospective
study was conducted at the Department of Surgery,
SKIMS Medical College, Srinagar, Kashmir, India.
The medical records of all the patients treated
for delayed presentation of PTDH from June 2010 to
May 2024 were retrieved from the databank.
Carter’s
classification criteria [5] concern the temporal
parameter of the development of PTDH and recognize
three phases: the acute phase (up to 14 days after
injury), the interval or latent phase when
patients may be asymptomatic, and the obstructive
phase when symptoms start appearing. The latter
two phases are collectively referred to as delayed
PTDH, and in this study, presentation in these
phases was the single inclusion criterion to be
fulfilled. The exclusion criteria included acute
PTDH and congenital diaphragmatic hernia.
This study did not
involve any invasive interventions but relied on a
retrospective analysis of stored data and was
approved by the departmental review committee.
Proper informed consent was sought from the
patients for publication the data and the
accompanying images, after assuring them of
privacy and confidentiality, under the Declaration
of Helsinki.
Results
The patient characteristics are depicted in Table
1 .
|
Table 1: Patient characteristics
of posttraumatic diaphragmatic hernia
|
|
Serial number
|
Gender
|
Age (y-year)
|
History (d- day, w -week,
m-month, y-year)
|
Type of index injury
|
Treatment of index injury
|
Interval since index injury (m-
month; y – year)
|
Site of hernia
|
Imaging
|
Surgical approach
|
Operation findings
|
Management
|
Postoperative phase &
follow-up
|
|
1
|
F
|
50
|
AP, Vom - 1 d
O/E
Decreased
BS at base of left lung
|
B (fall from height)
|
Co
|
5m
|
L
|
CXR: Elevated (L) hemidiaphragm
CECT: DH with collapse of ipsilateral
lung and mild pleural effusion
|
Lap
|
Herniated omentum and SI; diaphragm
defect 7 x 5 cm
|
Reduction of DH, mesh repair of
diaphragm, chest tube
|
Uneventful, no recurrence at 1 y
|
|
2
|
F
|
17
|
Recurrent episodes of AP - 2y. O/E
Decreased BS with audible bowel sounds at
base of left lung
|
B (fall from height)
|
Co
|
4y
|
L
|
CXR: Elevated left hemidiaphragm CECT:
diaphragmatic herniation of multiple small
intestine loops
|
Lap
|
Herniated SI; diaphragm defect 10 x 6 cm
|
Reduction of DH, mesh repair of diaphragm
|
Uneventful, no recurrence at 3 y
|
|
3
|
M
|
45
|
AP - 6m; Fever 1w
|
B (motor vehicle accident)
|
Co
|
5y
|
R
|
CXR- Elevated (R) dome of diaphragm
CECT-Scan- 6x5 cm defect in R
hemidiaphragm, (R) lung collapse
|
Lap
|
Herniated gangrenous omentum with
collapsed (R) lung; diaphragm defect 7 x 6
cm
|
Reduction & excision of gangrenous
omentum, primary diaphragm repair, chest
tube
|
Uneventful, no recurrence at 5 y
|
|
4
|
M
|
55
|
Chest discomfort, abdominal distension,
& bloating- 3m
|
B (workplace accident)
|
Co
|
6y
|
L
|
CXR: Elevated and distorted (L)
hemidiaphragm. NCCT- (L) Diaphragmatic
defect with herniated air-filled splenic
flexure.
|
Lap
|
Herniated splenic flexure and omentum;
diaphragm defect 5 x 3 cm
|
Reduction of DH, mesh repair of
diaphragm.
|
Uneventful postoperative phase but lost
to follow -up .
|
|
5
|
F
|
25
|
Recurrent episodes of AP - 1y
|
B (assault )
|
Co
|
7y
|
L
|
CXR: Elevated and distorted (L)
hemidiaphragm; bowel loops in chest. CECT:
Diaphragmatic herniation of transverse
colon
|
Lap
|
Herniated transverse colon; diaphragm
defect 7 x 3 cm
|
Reduction of DH, primary repair of
diaphragm
|
Uneventful, no recurrence at 5 y
|
|
6
|
F
|
58
|
AP and bloating – 1y, Shoulder pain – 6 m
|
P (workplace accident)
|
Laparotomy, splenectomy
|
4y
|
R
|
CXR: Elevated and distorted (R)
hemidiaphragm. CECT: Herniated greater
omentum and portion of intestine, minimal
lung collapse
|
Lap
|
Herniated greater omentum and portion of
transverse colon; diaphragm defect 5 x 4
cm
|
Reduction of DH, primary repair of
diaphragm
|
Uneventful, no recurrence at 1 y
|
|
7
|
F
|
14
|
AP, Vom -
2d
|
B (fall from height)
|
Co
|
7m
|
L
|
CXR: Elevated and distorted (L)
hemidiaphragm. CECT: diaphragmatic
herniation of SI
|
Lap converted to Open
|
Herniated transverse colon; diaphragm
defect 8 x 5 cm
|
Reduction of DH, primary repair of
diaphragm
|
Uneventful, no recurrence at 7 y
|
|
AP: Abdominal pain; Vom: Vomiting; B:
Blunt; P: Penetrating; Co : Conservative ;
L : Left ; R : Right ; DH : Diaphragmatic
Hernia ; SI: Small intestine ; Lap:
Laparoscopic ; BS : Breath sounds
|
There were 5 (71.4%)
females and 2 (28.6%) males, ranging in age from
14 years to 58 years (mean 37.7 years). The
clinical presentations of the patients included
abdominal pain (n = 7; 100%), nausea/vomiting (n =
2; 28.6%), abdominal bloating (n = 2; 28.6%),
chest discomfort/breathlessness (n = 1; 14.3%),
and shoulder pain (n = 1; 14.3%). Physical
examination revealed diminished breath sounds
(n-2; 28.6%) and audible bowel sounds (n-1; 14.3%)
over the affected hemithorax. Five cases (71.4%)
had chronic symptoms ranging from 3 months to 2
years. 2 (28.6%) cases presented acutely with
symptoms for 1 and 2 days, respectively. The
mechanism of index injury was blunt in 6 (85.7%)
cases who had been managed conservatively, and 1
(14.3%) case had a history of penetrating trauma,
managed by laparotomy with splenectomy. The
interval between index injury and presentation of
PTDH ranged from 5 months to 7 years (mean 4.6
years). Hernia was left sided in 5 (71.4%) and
right sided in 2 (28.6%) cases.
X-ray chest (with or
without plain X-ray abdomen) and CT scan
chest/abdomen were undertaken in all cases
(Figures 1A & 1B). CT scan was contrast
enhanced in 6 (85.7%) cases and non-contrast
enhanced in 1 (14.3%). These imaging modalities
revealed features suggestive of herniation of
viscera/bowel loops into the thorax. Once the
diagnosis of PTDH was confirmed, all the patients
underwent surgical operation, which entailed
reduction of hernia, repair of diaphragmatic
defect primarily with non-absorbable sutures (n =
5; 71.4%) or with mesh (n = 2; 28.6%), excision of
gangrenous omentum (n = 1; 14.3%), and tube
thoracostomy (n = 2; %). All the cases went
through an uneventful postoperative phase, and the
only postoperative complication was superficial
surgical site infection in 1 (14.3%) case. The
approach was laparoscopic in 6 (85.7%) cases, and
in 1 (14.3%) case, due to technical difficulties,
conversion to an open approach was undertaken. One
case was lost to follow-up, and there was no
recurrence in the remaining six cases at follow-up
ranging from 1 year to 7 years (3.7 years) as
determined by physical examination and imaging (
Figure 2).
|
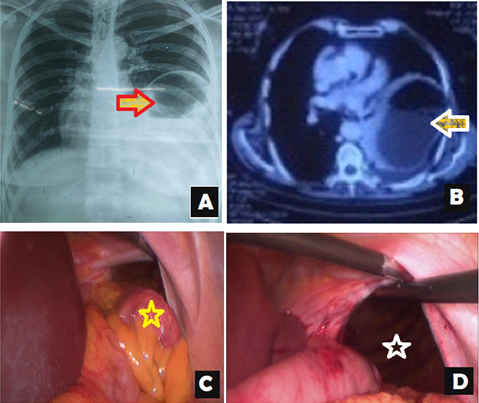
| Figure
1: (A) CXR Chest: Raised left diaphragm,
air fluid levels projecting into lower
half of left hemithorax & left
lower lung atelectasis (red arrow). (B)
Contrast enhanced CT scan Chest:
Intrathoracic herniation of hollow viscera
(white arrow) (C) Herniated splenic
flexure of colon (yellow star). (D)
Diaphragmatic defect after reduction of
herniated contents (white star).
|
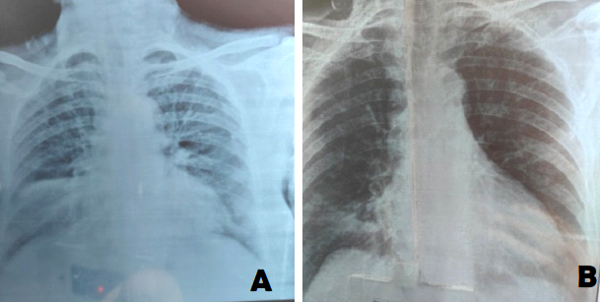 |
| Figure
2: Posttraumatic right diaphragmatic
hernia A: Preoperative Chest Xray B :
Chest Xray at one year follow up after
surgical operation. |
Discussion
Traumatic
diaphragmatic injury (TDI) is a rare condition
that occurs in approximately 0.5% to 5% of
abdominal trauma cases, with a ratio of 2:1 for
penetrating to blunt trauma [6]. They occur mostly
in the areas of potential weakness along
embryological points of fusion by a sudden
increase in the pleuroperitoneal pressure gradient
in thoracoabdominal trauma and result in the entry
of an abdominal viscera into the pleural cavity
[1, 7].
Historically,
Sennertus described it for the first time in 1541
when he performed an autopsy on a patient who had
died eight months after being shot and found
strangulation of the colon that had herniated
through the diaphragmatic defect [8]. Ambroise
Pare later documented PTDH in an artillery
commander in 1579, and Riolfi made the first
successful repair in 1886 [9]. The delay in
presentation can be explained because of the
pattern of emergence as below:
i. After being
devitalized due to trauma, the diaphragmatic
muscle becomes inflamed and heals by developing a
weak scar that eventually breaks down, resulting
in a defect that progressively extends in size
through radial pulling during breathing. [10].
ii. Sometimes a
defect is produced at the time of injury, but
because there hasn't been a herniation of
intra-abdominal viscera into the chest cavity, the
symptoms don't show up right away, or they get
masked up by more serious, potentially fatal
injuries [11].
The symptoms with
which the patients presented in this series
included abdominal pain (n = 7; 100%),
nausea/vomiting (n = 2; 28.6%), abdominal bloating
(n = 2; 28.6%), chest discomfort/breathlessness (n
= 1; 14.3%), and shoulder pain (n = 1; 14.3%).
None of the cases reported with hemodynamic
instability or respiratory compromise, though
cases are reported in literature where missed
hernias had manifested many months or even years
later as complications such as intestinal
obstruction, perforation, or ischemia with
morbidity and mortality rates as high as 30% and
10%, respectively [12-13]. Acute tension
viscerothorax is a manifestation where herniated
viscera into the thoracic cavity produces
hemodynamic compromise but without perforation
[14-15]. Tension faecopneumothorax (TFP) is a rare
and potentially lethal presentation of PTDHs. It
is a condition where herniated gut perforates,
releasing gas and feces-contaminated fluids into
the pleural cavity, creating an intrapleural
pressure that exceeds the atmospheric pressure,
thereby leading to adverse effects, which include
mediastinal shift, kinking of the great vessels,
reduced venous return, and cardiovascular collapse
[16-18].
The interval between
the initial trauma and the clinical presentation
with PTDH ranged from 5 months to 7 years (mean
4.6 years) in this series. When a patient presents
years or decades later, it may be challenging to
diagnose them because they may have forgotten the
episode of trauma, particularly if managed
conservatively, or else the healthcare provider
may not have enough awareness to connect the acute
symptoms to the index injury of the past [16].
Singh et al. [19] and Faul [20] have reported
cases of PTDH that presented 50 years and 40
years, respectively, after the traumatic event.
Hariharan et al. [21] reported a 65-year-old male
with splenic herniation into the left hemithorax,
causing fundal varices leading to hematemesis and
melena 28 years after the penetrating injury.
Popovic et al. [22] have presented a case where
symptoms due to PTDH appeared 26 years after the
index injury. The symptoms (epigastric pain,
meteorism, nausea, and vomiting) were interpreted
as acute alcoholic gastritis. The condition of the
patient, however, deteriorated, and on evaluation,
the diagnosis of gastrothorax was made.
In this series, PTDH
was left sided in 5 (71.4%) and right sided in 2
(28.6%) cases. This proportion concurs with the
data in the literature that shows the predominance
of hernias on the left side and is attributed to
the protective nature of the liver on the right,
the increased strength of the right part of the
diaphragm, and the weakness of the left
hemidiaphragm at embryonic points of fusion
[23-24]. The location of hernia influences the
nature of clinical features. Left-sided hernias
tend to present with obstructive gastrointestinal
symptoms, recurrent thoracoabdominal pain,
dyspnea, postprandial fullness, and vomiting [24].
Right-sided hernia is commonly limited to
respiratory difficulties, and the liver tends to
hinder the further visceral herniation due to its
bulk [25].
X-ray chest and CT
scan were the major imaging modalities utilized in
all the patients in this series. Imaging has a
significant role in the management of PTDH by
revealing features including elevation of the
hemidiaphragm, radiopacities in the hemithorax,
and displacement of the mediastinum towards the
contralateral side [8, 25]. Successful diagnosis
requires a high index of suspicion, but if
visceral herniation has occurred, diagnosis can be
made from the chest radiograph in 90% of the
patients [26-27].
In this series, the
approach adopted for surgical management was
laparoscopic in 6 (85.7%) cases, and in 1 (14.3%)
case, due to technical difficulties, conversion to
an open approach was undertaken. In literature,
different approaches have been reported, including
laparotomy, thoracotomy, combined laparotomy and
thoracotomy, laparoscopy, and video-assisted
thoracic surgery, depending on the type of injury
(acute or chronic), the laterality of the injury,
the surgeon's experience, and the availability of
equipment [8]. The literature recommends the use
of nonabsorbable suture material and that the
running or interrupted sutures can be used to
repair diaphragmatic abnormalities with comparable
efficacy [28]. The laparoscopic approach has been
found to be a safe treatment by several authors
due to its minimally invasive nature.
Conclusion
Post-traumatic diaphragmatic hernias with delayed
presentation are rarely encountered and can be
challenging for surgeons. A high index of
suspicion is required for diagnosis in patients
who have a past history of thoracoabdominal
trauma. Wrong diagnosis and delay in management
can lead to morbidity and mortality .The patients
discharged after thoracoabdominal trauma need
radiographical follow-ups to detect diaphragmatic
hernias at an earlier stage. Management is
surgical, and laparoscopic approach is successful
in most situations, though the approach depends
upon the patient characteristics, skill of the
surgeons, and the availability of equipment.
Acknowledgements
The patients' consent to the use of their photos
for scholarly purposes is acknowledged by the
authors. This study does not have any financial
sources, and there are no conflicts of interest.
The article was prepared with input from each
author.
References
- Lu J, Wang B, Che X, Li X, Qiu G, He S, Fan L.
Delayed traumatic diaphragmatic hernia: A
case-series report and literature review. Medicine
(Baltimore) 2016 Aug;95(32):e4362. doi:
10.1097/MD.0000000000004362.
- Al-Saqqa R, Sabouni R, Jarad L, Abbas N. A
delayed post-operative diaphragmatic hernia with
hemothorax due to a strangulated stomach. J
Surg Case Rep. 2020 Dec
28;2020(12):rjaa515. doi: 10.1093/jscr/rjaa515.
- Yusufi MA, Uneeb M, Nazir I, Rashid F.
Laparoscopic Repair of Blunt Traumatic
Diaphragmatic Hernia. Cureus. 2023 Sep
26;15(9):e46017. doi: 10.7759/cureus.46017.
- Morgan BS, Watcyn-Jones T, Garner JP.
Traumatic diaphragmatic injury. J R Army Med
Corps. 2010 Sep;156(3):139-44. doi:
10.1136/jramc-156-03-02.
- Carter BN, Giuseffi J, Felson B. Traumatic
diaphragmatic hernia. Am J Roentgenol Radium
Ther. 1951 Jan;65(1):56-72. PMID:
14799666.
- Reitano E, Cioffi SPB, Airoldi C, Chiara O, La
Greca G, Cimbanassi S. Current trends in the
diagnosis and management of traumatic
diaphragmatic injuries: A systematic review and
a diagnostic accuracy meta-analysis of blunt
trauma. Injury. 2022;53(11):3586-3595.
doi: 10.1016/j.injury.2022.07.002
- El Bakouri A, El Karouachi A, Bouali M, El
Hattabi K, Bensardi FZ, Fadil A. Post-traumatic
diaphragmatic rupture with pericardial
denudation: A case report. Int J Surg Case
Rep. 2021; 83:105970.
doi:10.1016/j.ijscr.2021.105970
- Okyere I, Mensah S, Singh S, Okyere P, Kyei I,
Brenu SG. Surgical management of traumatic
diaphragmatic rupture: ten-year experience in a
teaching hospital in Ghana. Kardiochir
Torakochirurgia Pol. 2022;19(1):28-35.
doi:10.5114/kitp.2022.114552
- Schwindt WD, Gale JW. Late recognition and
treatment of traumatic diaphragmatic hernias. Arch
Surg. 1967; 94(3):330-334.
doi:10.1001/archsurg.1967.01330090024006
- Yucel M, Bas G, Kulalı F, et al. Evaluation of
diaphragm in penetrating left thoracoabdominal
stab injuries: The role of multislice computed
tomography. Injury.
2015;46(9):1734-1737.
doi:10.1016/j.injury.2015.06.022
- Vermillion JM, Wilson EB, Smith RW. Traumatic
diaphragmatic hernia presenting as a tension
fecopneumothorax. Hernia.
2001;5(3):158-160. doi:10.1007/s100290100022
- Shaban Y, Elkbuli A, McKenney M, Boneva D.
Traumatic diaphragmatic rupture with
transthoracic organ herniation: a case report
and review of literature. Am J Case Rep.
2020;21: e919442. doi:10.12659/AJCR.919442
- Tessely H, Journé S, Therasse A, Hossey D,
Lemaitre J. A case of colon necrosis resulting
from a delayed traumatic diaphragmatic hernia. J
Surg Case Rep. 2020 Jun
17;2020(6):rjaa101. doi: 10.1093/jscr/rjaa101.
- Ahn S, Kim W, Sohn CH, Seo DW. Tension
viscerothorax after blunt abdominal trauma: a
case report and review of the literature. J
Emerg Med. 2012;43(6): e451-e453. doi:
10.1016/j.jemermed.2011.05.084
- Ekim H, Tuncer M, Ozbay B. Tension
viscerothorax due to traumatic diaphragmatic
rupture. Annals of Saudi Medicine,
2008;28(3), 207–208. doi:
10.5144/0256-4947.2008.207.
- Chern TY, Kwok A, Putnis S. A case of tension
faecopneumothorax after delayed diagnosis of
traumatic diaphragmatic hernia. Surg Case
Rep. 2018;4(1):37. doi:
10.1186/s40792-018-0447-y.
- Ramdass MJ, Kamal S, Paice A, Andrews B.
Traumatic diaphragmatic herniation presenting as
a delayed tension faecopneumothorax. Emerg
Med J. 2006;23(10): e54.
doi:10.1136/emj.2006.039438
- Kafih M, Boufettal R. A late post-traumatic
diaphragmatic hernia revealed by a tension
fecopneumothorax (a case report). Rev Pneumol
Clin. 2009;65(1):23-6. doi:
10.1016/j.pneumo.2008.10.004.
- Singh S, Kalan MM, Moreyra CE, Buckman RF Jr.
Diaphragmatic rupture presenting 50 years after
the traumatic event. J Trauma. 2000
Jul;49(1):156-9. doi:
10.1097/00005373-200007000-00025.
- Faul JL. Diaphragmatic rupture presenting
forty years after injury. Injury. 1998
Jul;29(6):479-80. doi:
10.1016/s0020-1383(98)00082-5.
- Hariharan D, Singhal R, Kinra S, Chilton A.
Post traumatic intra thoracic spleen presenting
with upper GI bleed!--a case report. BMC
Gastroenterol. 2006 Nov 28;6:38. doi:
10.1186/1471-230X-6-38.
- Popovic T, Nikolic S, Radovanovic B, Jovanovic
T. Missed Diaphragmatic Rupture and Progressive
Hepatothorax, 26 Years after Blunt Injury. Eur
J Trauma 2004; 30:43–46.
https://doi.org/10.1007/s00068-004-1327-7
- da Costa KG, da Silva RTS, de Melo MS, Pereira
JTS, Rodriguez JER, de Souza RCA, de Oliveira
Medeiros IA. Delayed diaphragmatic hernia after
open trauma with unusual content: Case report. Int
J Surg Case Rep. 2019;64:50-53.
doi:10.1016/j.ijscr.2019.08.030
- Christie DB, Chapman J, Wynne JL, Ashley DW.
Delayed right-sided diaphragmatic rupture and
chronic herniation of unusual abdominal
contents. J Am Coll Surg. 2007
Jan;204(1):176. doi:
10.1016/j.jamcollsurg.2006.05.007.
- Testini M, Girardi A, Isernia RM, De Palma A,
Catalano G, Pezzolla A. Emergency surgery due to
diaphragmatic hernia: Case series and review. World
J Emerg Surg. 2017;12:23. doi:
10.1186/s13017-017-0134-5.
- Maddox PR, Mansel RE, Butchart EG. Traumatic
rupture of the diaphragm: a difficult diagnosis.
Injury. 1991 Jul;22(4):299-302. doi:
10.1016/0020-1383(91)90010-c.
- Peer SM, Devaraddeppa PM, Buggi S. Traumatic
diaphragmatic hernia-our experience. Int J
Surg. 2009 Dec;7(6):547-9. doi:
10.1016/j.ijsu.2009.09.003.
- Necke K, Heeren N, Mongelli F, FitzGerald M,
Fornaro J, Minervini F, Metzger J, Gass J M.
Faecopneumothorax caused by perforated
diaphragmatic hernia. Case Rep Surg.
2020; 2020:8860336. doi:10.1155/2020/8860336.
|



















