|
Introduction
According
to a Lancet Diabetes study published in 2022,
India has surpassed China as the country with the
largest number of people with diabetes (1).
Diabetes is linked to nearly every chronic
disease. There is a high prevalence of Diabetes
and related non-communicable diseases (NCDs) in
India, leading to a significant population at risk
for cardiovascular diseases and chronic
complications of diabetes, such as kidney, foot
and eye diseases, according to the Indian Council
of Medical Research-India Diabetes (ICMR-INDIAB)
study (2,3).
Maintaining good
glycaemic control is vital for preventing and
delaying the progression of these
complications(4). Following diet modifications and
lifestyle changes, the initial recommended therapy
for type 2 diabetes mellitus (T2DM) is metformin.
Based on baseline HbA1c at diagnosis, there are
several other alternative oral antidiabetics,
which include sulfonylureas (SU), glucagon-like
peptide (GLP-1), di-peptidyl peptidase-4
inhibitors (DPP-4i), sodium glucose
co-transporters-2 inhibitors (SGLT2i) and alpha
glucosidase inhibitors (AGIs). Despite the
availability and widespread use of anti-diabetic
drugs, the poor achievement of glycaemic targets
suggests insufficient monitoring and follow-up. A
recent study on diabetes prevalence in India,
published in Diabetes Research and
Clinical Practice, observed that nearly half of
the tested population exhibited abnormal glucose
levels when analysing their HbA1c test results(5).
Regular follow-ups with healthcare providers are
essential for achieving glycemic control and
preventing T2DM associated complications(6). It is
therefore essential to focus antidiabetic
treatment approaches not only on glycemic control
but also on preventing diabetes-related
complications and comorbidities without triggering
hypoglycaemic episodes, weight gain or
cardio-renal toxicity. Two classes of oral
hypoglycaemic agents that meet the above criteria
are sodium-glucose cotransporters-2 inhibitors
(SGLT2i) and dipeptidyl peptidase-4 inhibitors
(DPP-4i)(7,8).
These newer classes
of oral anti-diabetic agents SGLT2i and DPP-4i,
were approved in India a decade ago. Both these
classes have received much attention owing to
their cardio-renal benefits, weight loss and fewer
incidences of hypoglycaemic episodes unlike the
traditional anti-diabetic agents(9). SGLT2i
(dapagliflozin, canagliflozin, empagliflozin)
block the sodium-glucose transport proteins,
preventing the reabsorption of 90% of glucose in
the glomerulus and increasing glucose loss through
urine. While selective DPP-4i (sitagliptin,
vildagliptin, linagliptin) reduce the fasting
glucose and post-meal spikes by preventing the
degradation of glucose-dependent insulinotropic
polypeptide (GDIP) and glucagon-like
peptide1(GLP-1)(4). These two newer classes of
anti-diabetic agents are preferred for managing
T2DM patients with complications, according to
guidelines from the American Diabetes Association
(ADA) and Kidney Disease Improving Global Outcomes
(KDIGO) guidelines(10). Combining SGLT2i or DPP-4i
with metformin is an effective strategy to improve
the glucose-lowering effect. However, triple
therapy with metformin, SGLT2i and DPP-4i has
shown potential for significant reduction in HbA1c
levels, fasting and postprandial blood glucose,
body weight and blood pressure (11-13). Given the
increasing impact of diabetes, positioning it as a
pandemic in making, and the availability of newer
anti-diabetic agents in India, there has been a
significant shift in prescribing patterns of
anti-diabetic drugs. This study aimed to assess
the real-world prescribing trends of SGLT2i and
DPP-4i stratified by their HbA1c values in T2DM
patients with complications.
Materials and Methods
This was a
prospective cross-sectional observational analysis
of antidiabetic prescription patterns in Kerala,
India, conducted between October 2023 and December
2024. Patient records of individuals diagnosed
with T2DM and complications who visited a tertiary
care hospital were utilised for the study. The
Ethics committee of Karuna Medical College and
Hospital, Palakkad, approved the study protocol.
Patients aged >40 years with T2DM and
associated complications, with at least 1 HbA1c
laboratory result and who were prescribed
antidiabetic agents between 2023 and 2024, were
included. Patients with type 1 diabetes,
gestational diabetes and end-stage kidney disease
were excluded. Our primary objective was to
compare patients who received and did not receive
DPP-4i (teneligliptin, vildagliptin, sitagliptin
or linagliptin) or SGLT2i (empagliflozin or
dapagliflozin) treatment along with the
conventional classes of antidiabetic agents
(metformin, SU and Insulin) throughout the study
period. A subgroup analysis was conducted,
categorising patients into three distinct cohorts,
stratified based on their HbA1c levels; controlled
(HbA1c <7.5%), above-target (HbA1c 7.5%-9%),
and elevated (HbA1c > 9%). The demographic
characteristics such as age, sex, HbA1c values,
diabetes-specific complications, co-morbidities
and use of other antidiabetic drugs, were
tabulated for these 3 cohorts. The study also
examined the pattern of therapy in relation to
patient’s HbA1c levels and factors associated with
prescribing newer antidiabetic agents.
Statistical
Analysis:
Standardized
differences were used to evaluate balance across
groups in terms of demographic characteristics,
HbA1c levels and comorbidities and
treatment-related factors such as the number of
glucose-lowering drugs and the use of specific
anti-diabetic agents. This approach ensured a
consistent comparison of baseline characteristics
and treatment patterns between patients receiving
newer antidiabetic agents (SGLT2i and DPP4i) and
those on traditional therapies (Metformin and
Sulfonylureas) across different HbA1c categories
(<7.5%, 7.5%-9%, >9%). Categorical
variables, including comorbidities and prescribing
patterns, were compared using chi-square tests.
Statistical significance was determined at a
p-value threshold of 0.05, focusing on identifying
patterns in prescribing practices and glycemic
control among the study population. The data was
analysed using IBM SPSS 22 software.
Results
Of the 260 eligible
patients (mean [SD] age, 63.7[12.4] years; 54.6%
male patients) with T2DM identified, 36.5% of
diabetic patients initiated treatment with newer
antidiabetic agents and 84.6% initiated
traditional antidiabetic agents. 49.6% had
controlled HbA1c value, 33.4% above target levels
and only 16.9% of patients had uncontrolled
glycaemic levels. Table 1 evaluates newer (SGLT2i,
DPP-4i) and traditional (Metformin, SU)
antidiabetic agents across HbA1c ranges (<7.5%,
7.5%-9%, >9%), analysing demographic, clinical,
and treatment-related factors through standardized
differences (St. Diff). Age and HbA1c levels were
well-balanced across groups (St. Diff <0.4),
but gender showed a notable imbalance in the HbA1c
>9% group for newer antidiabetic agents (St.
Diff = 1). Male patients had a higher rate of
using newer antidiabetic agents (20%) compared to
female patients (16.5%). The most common
comorbidities were hypertension (75.7%), coronary
artery disease (46.3%) and nephropathy (46.3%).
Comorbidities like nephropathy and CAD
demonstrated moderate to high imbalances,
particularly in the HbA1c <7.5% group (e.g.,
nephropathy St. Diff = -0.96, CAD St. Diff =
0.89). These complications were prevalent among
individuals with HbA1c levels between 7.5% and 9%.
DPP-4i was more commonly prescribed for diabetes
related complications like nephropathy (60.7%),
while patients with coronary artery disease were
more frequently prescribed SGLT2i (66.6%). In
traditional antidiabetic cohorts, hypertension in
the HbA1c >9% group showed significant
imbalance (St. Diff = -0.91). A higher percentage
of males was prescribed with traditional agents
(53.6% vs 46.3%). Nephropathy and coronary artery
disease were the most prevalent diabetes-related
comorbidities, with metformin being the mainstay
treatment in these patients. Also, patients with
HbA1c levels ranging from 7.5% to 9% frequently
exhibited coronary artery disease. For these
patients, SGLT2i and DPP-4i were prescribed
equally as adjunct therapies alongside traditional
antidiabetic agents (13.6% vs 14.5%). Treatment
intensity, indicated by the number of
glucose-lowering drugs, was higher in patients
with HbA1c >9%, with imbalances reaching -0.93
for newer antidiabetic agents. Insulin use was
more frequent in higher HbA1c groups but displayed
smaller differences. Overall, newer agents were
more commonly prescribed in patients with complex
comorbidities and higher HbA1c levels, reflecting
tailored prescribing patterns.
|
Table 1: Baseline characteristics
of patients initiating SGLT2i vs DPP-4i
therapy overall and stratified by HbA1c
levels
|
|
HbA1c <7.5%
|
HbA1c 7.5%-9%
|
HbA1c >9%
|
|
| Newer
anti-diabetic agents prescribed |
|
SGLT2i
(n =17)
|
DPP4i
(n =24)
|
St. Diff
|
SGLT2i (n =15)
|
DPP4i
(n =28)
|
St. Diff
|
SGLT2i (n =12)
|
DPP4i (n =6)
|
St. Diff
|
Overall Population (n =95)
|
|
Age, mean (SD)
|
65 (11.64)
|
67.54(10.7)
|
-0.23
|
67.2(10.8)
|
63.46(12.67)
|
0.32
|
56.58(12.88)
|
55(13.74)
|
0.12
|
63.70(12.47)
|
|
Male, n (%)
|
11(64.71)
|
11(45.83)
|
0.54
|
10(66.67)
|
15(53.57)
|
0.38
|
6(50)
|
5(83.33)
|
-1
|
52
|
|
Female, n (%)
|
6(35.29)
|
13(54.17)
|
-0.54
|
5(33.33)
|
13(46.43)
|
-0.38
|
6(50)
|
1(16.67)
|
1
|
43
|
|
Laboratory data
|
|
HbA1c value, % mean (SD)
|
6.33(11.64)
|
6.4(0.69)
|
-0.01
|
8.10(0.29)
|
8.11(12.67)
|
-0.001
|
10.38(0.58)
|
10.33(0.93)
|
0.065
|
7.78 (1.49)
|
|
Diabetes related comorbidities, n
(%)
|
|
Nephropathy
|
2(11.76)
|
10(41.67)
|
-0.96
|
6(40)
|
17(60.71)
|
-0.59
|
4(33.33)
|
1(16.67)
|
0.54
|
40
|
|
Neuropathy
|
-
|
-
|
|
-
|
1(3.57)
|
-0.2
|
1(8.33)
|
-
|
|
1
|
|
Retinopathy
|
-
|
-
|
|
-
|
-
|
|
-
|
|
|
|
|
CAD
|
11(64.71)
|
8(33.33)
|
0.89
|
10(66.67)
|
10(35.71)
|
0.88
|
6(50)
|
2(33.33)
|
0.48
|
44
|
|
CVA
|
1(5.88)
|
3(12.50)
|
-0.32
|
2(13.33)
|
4(14.29)
|
-0.04
|
1(8.33)
|
2(33.33)
|
-0.87
|
12
|
|
Other comorbidities, n (%)
|
|
Hypertension
|
12(70.59)
|
23(95.83)
|
-0.96
|
11(73.33)
|
20(71.43)
|
0.06
|
5(41.67)
|
3(50)
|
-0.24
|
72
|
|
Hepatitis
|
4(23.53)
|
-
|
0.79
|
1(6.67)
|
3(10.71)
|
-0.2
|
-
|
1(16.67)
|
-0.85
|
9
|
|
COPD
|
2(11.76)
|
1(4.17)
|
0.4
|
1(6.67)
|
|
0.53
|
1(8.33)
|
-
|
0.59
|
5
|
|
BPH
|
2(11.76)
|
2(8.33)
|
0.16
|
3(20.00)
|
2(7.14)
|
0.53
|
-
|
1(16.67)
|
-0.85
|
10
|
|
Diabetes treatment
|
|
No. glucose lowering drugs, mean (SD)
|
2.23(1.03)
|
2.16(1.09)
|
0.07
|
2.8(1.2)
|
2.35(1.09)
|
0.39
|
3.16(0.93)
|
3.83(0.4)
|
-0.93
|
2.36(1.07)
|
|
Metformin, n (%)
|
9(52.94)
|
11(45.83)
|
0.2
|
9(60.00)
|
11(39.29)
|
0.59
|
9(75)
|
5(83.33)
|
-0.29
|
54
|
|
SU (II Gen), n (%)
|
6(35.29)
|
7(29.17
|
0.19
|
6(40.00)
|
8(28.57)
|
0.34
|
7(58.33)
|
4(66.67)
|
-0.24
|
38
|
|
Insulin, n (%)
|
4(23.53)
|
5
|
0.09
|
7(46.67)
|
13(46.43)
|
0.01
|
7(58.33)
|
3(50)
|
0.24
|
36
|
|
Baseline characteristics of
patients initiated with metformin vs
sulfonylureas therapy overall and
stratified by HbA1c levels
|
|
HbA1c <7.5%
|
HbA1c 7.5%-9%
|
HbA1c >9%
|
|
| Traditional
anti-diabetic agents prescribed |
|
Metformin (n =96)
|
SU (n =46)
|
St. Diff
|
Metformin (n =62)
|
SU (n =37)
|
St. Diff
|
Metformin (n =46)
|
SU (n =26)
|
St. Diff
|
Overall Population (n =220)
|
|
Age, mean (SD)
|
63.59(12.3)
|
63.56(11.53)
|
0.03
|
65.37(11.94)
|
65.70(13.37)
|
-0.03
|
58.54(11.72)
|
59.34(11.15)
|
-0.07
|
63.68(12.49)
|
|
Male, n (%)
|
48(50)
|
23(50)
|
0
|
33(53.23)
|
21(56.76)
|
-0.1
|
21(45.65)
|
13(50)
|
-0.12
|
118
|
|
Female, n (%)
|
48(50)
|
23(50)
|
0
|
29(46.67)
|
16(43.24)
|
0.1
|
25(54.35)
|
13(50)
|
0.12
|
102
|
|
Laboratory data
|
|
HbA1c value, % mean (SD)
|
6.19(0.75)
|
6.36(0.73)
|
-0.23
|
8.11(0.69)
|
8.28(0.51)
|
-0.28
|
10.11(1.82)
|
10.74(0.98)
|
-0.43
|
7.66(1.81)
|
|
Diabetes related comorbidities, n
(%)
|
|
Nephropathy
|
18(18.75)
|
6(13.04)
|
0.22
|
16(25.8)
|
8(21.62)
|
0.14
|
8(17.39)
|
4(15.38)
|
0.08
|
47
|
|
Neuropathy
|
1(1.04)
|
2(4.35)
|
-0.29
|
3(4.84)
|
4(10.81)
|
-0.31
|
6(13.04)
|
4(15.38)
|
-0.09
|
11
|
|
Retinopathy
|
2(2.08)
|
1(2.17)
|
-0.01
|
-
|
1(2.70)
|
-0.33
|
6(13.04)
|
2(7.69)
|
0.25
|
9
|
|
CAD
|
12(12.50)
|
10(21.74)
|
-0.35
|
19(30.65)
|
11(29.73)
|
0.03
|
15(32.61)
|
8(30.77)
|
0.06
|
52
|
|
CVA
|
8(8.33)
|
6(13.04)
|
-0.22
|
10(16.13)
|
5(13.51)
|
0.1
|
7(15.22)
|
5(19.23)
|
-0.15
|
27
|
|
Other comorbidities, n (%)
|
|
Hypertension
|
66(68.75)
|
29(63.04)
|
0.17
|
39(62.90)
|
22(59.46)
|
0.1
|
6(13.04)
|
14(53.85)
|
-0.91
|
137
|
|
Hepatitis
|
11(11.46)
|
10
|
-0.39
|
6(9.68)
|
3(8.11)
|
0.08
|
-
|
1(3.85)
|
-0.4
|
27
|
|
COPD
|
2(2.08)
|
3
|
-0.31
|
2(3.23)
|
-
|
0.36
|
-
|
-
|
|
6
|
|
BPH
|
3(3.13)
|
3
|
-0.22
|
6(9.68)
|
1(2.70)
|
0.41
|
1(2.17)
|
2(7.69)
|
-0.36
|
18
|
|
Diabetes treatment
|
|
No. glucose lowering drugs, mean (SD)
|
1.88(0.91)
|
2.37(0.98)
|
-0.52
|
2.32(0.88)
|
2.59(0.98)
|
-0.29
|
2.63(1.08)
|
3.15(0.83)
|
-0.54
|
2.18(0.98)
|
|
SGLT2i, n (%)
|
9(9.38)
|
6
|
-0.16
|
9(14.52)
|
6(16.22)
|
-0.07
|
11(23.91)
|
7(26.92)
|
-0.1
|
30
|
|
DPP4i , n (%)
|
11(11.46)
|
7
|
-0.16
|
11(17.74)
|
8(21.62)
|
-0.14
|
6(13.04)
|
4(15.38)
|
-0.09
|
32
|
|
Abbreviations: DPP-4i, dipeptidyl
peptidase 4 inhibitors; SGLT2i, sodium
glucose co transporter 2 inhibitor; HbA1c,
Glycated hemoglobin; CAD, coronary artery
disease; CVA, cerebrovascular accident;
SU, sulfonylureas; COPD, chronic
obstructive pulmonary disease; BPH, benign
prostatic hyperplasia. Data are expressed
as number(percentage), mean+SD, St.Diff,
standardised differences, ie the
difference in mean divided by the pooled.
|
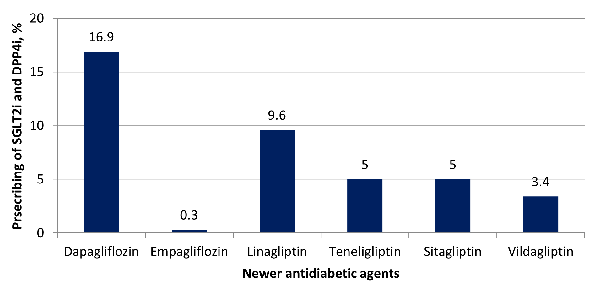
Utilisation percentage of newer
antidiabetic medication
Figure 1 summarises
the percentage usage of newer antidiabetic agents.
Of the 260 prescriptions, the percentage of SGLT2i
and DPP-4i prescriptions were as follows: 16.9%
for Dapagliflozin, 0.38% for empagliflozin, 9.6%
for linagliptin, 5% each for sitagliptin and
teneligliptin and 3.4% for Vildagliptin. This
distribution indicates that Dapagliflozin and
Linagliptin are the most preferred agents among
the newer antidiabetic drugs, likely reflecting
prescribing trends influenced by efficacy, safety
profiles, or patient-specific factors. The study
reveals that SGLT2i and DPP-4i are not widely
prescribed. Despite patients being diagnosed with
T2DM and associated complications, only a few
patients received these newer agents, hinting at a
lack of adherence to the latest treatment
guidelines as per ADA.
|
|
Figure
1: Patterns of Newer Anti-Diabetic
Agents used: SGLT2i and DPP-4i
distribution.
|
Antidiabetic treatment pattern stratified
by HbA1c status
Further analysis of
treatment patterns revealed diabetic patients
received treatments ranging from monotherapy to
quadruple therapy. Table 2 presents the
distribution of patients across various
antidiabetic therapy regimens and their
corresponding mean HbA1c levels with 95%
confidence intervals. Metformin monotherapy is the
most commonly used regimen (17.69%) and is
associated with the lowest mean HbA1c (6.48%),
indicating better glycemic control. Patients
prescribed with dual therapy of metformin and
sulfonylureas shows moderate HbA1c levels (7.76%).
In contrast, combination therapies, particularly
triple or quadruple regimens, are less common and
show higher mean HbA1c values, such as 8.81% in
the metformin, sulfonylureas, and SGLT2i triple
therapy group, demonstrating their preference in
patients with more challenging glycemic level. The
variability in HbA1c levels within regimens, as
indicated by wider confidence intervals, may
reflect differences in response to therapy
depending upon the HbA1c status. These findings
indicate that patients exhibiting higher levels of
glycated haemoglobin were prescribed newer
antidiabetic agents alongside traditional
treatment.
|
Table 2: Pattern of Antidiabetic
Therapy Regimens and Their Corresponding
HbA1c levels.
|
|
Antidiabetic combinations
|
HbA1c%
|
|
Number (%) of patients corresponding to
HbA1c value
|
Mean (95% CI)
|
|
Metformin monotherapy
|
46 (17.69)
|
6.48(6.01, 6.95)
|
|
Sulfonylureas monotherapy
|
13 (5)
|
6.64(6.01, 7.27)
|
|
SGLT2i monotherapy
|
8 (3.08)
|
7.14(6.38, 7.89)
|
|
DPP4i monotherapy
|
14 (5.38)
|
7.06(6.48,7.63)
|
|
Metformin plus sulfonylureas dual therapy
|
28 (10.77)
|
7.76(6.99, 8.54)
|
|
Metformin plus sulfonylureas plus DPP4i
triple therapy
|
11 (4.23)
|
8.16(7.19, 9.19)
|
|
Metformin plus sulfonylureas plus SGLT2i
triple therapy
|
13 (5)
|
8.81(7.68,9.93)
|
|
Metformin plus sulfonylureas plus Insulin
triple therapy
|
25 (9.62)
|
8.65(7.88, 9.43
|
|
Metformin plus sulfonylureas plus Insulin
plus SGLT2i or DPP4i quadruple therapy
|
7 (2.69)
|
8.64(7.41, 9.88)
|
|
Metformin plus sulfonylureas plus DPP4i
plus SGLT2i quadruple therapy
|
3 (1.15)
|
6.8(3.94, 9.67
|
Variation in prescribing pattern by age,
sex and prescriber speciality
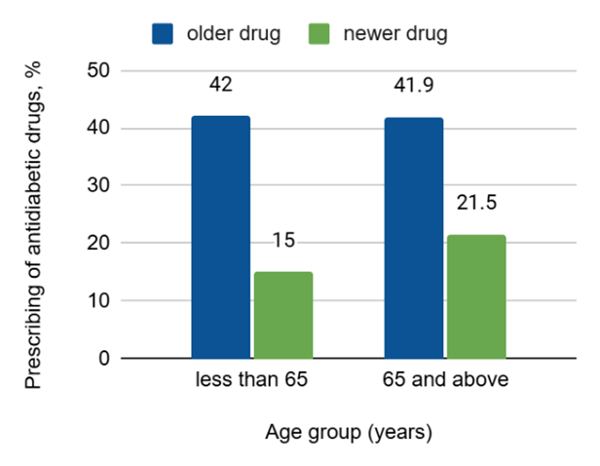
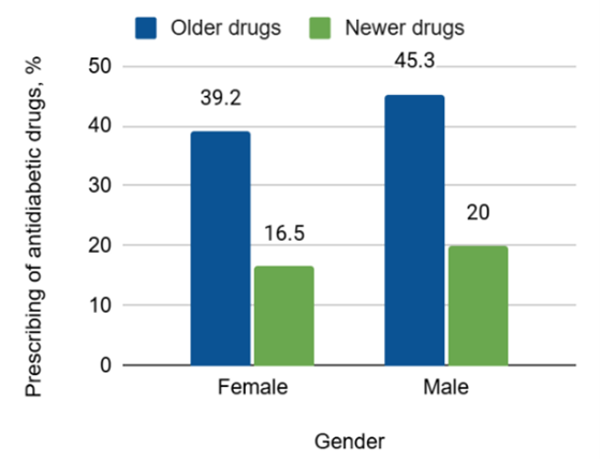
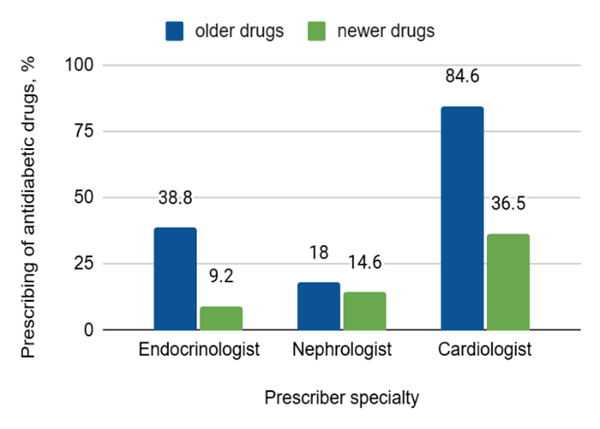
The prescribing
patterns of older and newer antidiabetic drugs
(SGLT2i and DPP4i) varied based on age, gender,
and prescriber speciality. While patients aged ≥65
years received newer drugs more frequently (21.5%)
compared to those <65 years (15%), this
difference was not statistically significant (p
= 0.182) (Figure 2a). Similarly, no significant
gender-based difference was observed, with males
(20%) and females (16.5%) receiving newer drugs at
comparable rates (p = 0.9548) (Figure
2b). Prescriber speciality showed a significant
impact (p = 0.00038). Endocrinologists
predominantly prescribed older drugs (38.8%),
while Nephrologists showed a relatively balanced
pattern (18% vs. 14.6%), and Cardiologists
demonstrated the highest shift toward newer drugs,
with 36.5% of their prescriptions being newer
agents, although older drugs remained dominant at
84.6%. These trends indicate that cardiologists
were more likely to adopt newer therapies compared
to endocrinologists and nephrologists, reflecting
variations in prescribing practices within
specialities (Figure 2c)
|
| Fig
2a: Age wise Prescribing Patterns
|
|
| Fig 2b: Gender-Wise
Prescribing Patterns |
|
| Fig 2c: Prescribing
Patterns among prescriber speciality |
Discussion
We collected medical
records between 2023 to 2024 to compare
antidiabetic prescribing patterns among patients
with T2DM and associated complications. Despite
evidence from landmark trials demonstrating the
cardiorenal benefits of SGLT2i and DPP-4i, their
prescribing remained limited during our study
period(14). In real-world settings, we observed
DPP-4i (22.3%) and SGLT2i (16.9%), were the third
and fourth most commonly prescribed anti-diabetic
medication after metformin (78.4%) and SU (41.9%).
A similar trend was observed by H Y. Chang et
al., with SGLT2i being the fourth most
commonly prescribed drug after metformin, DPP-4i
and SU(15). Mahtta et al., also observed
a similar trend among T2DM patients, with only
14.9% of patients receiving SGLT2i(16).
Metformin has
consistently been the first-line therapy
prescribed regardless of whether T2DM patients had
complications or not. In line with our study, the
DAPA-HF trial and ASIAN-HF registry also
identified metformin as the most commonly
prescribed antidiabetic agent(17,18). This
preference is likely due to metformin’s
well-established safety profile in T2DM patients
compared to other antidiabetic agents. Despite
recommendations to avoid its use in patients with
severe renal insufficiency, metformin is still
being prescribed to individuals with advanced
chronic kidney disease (CKD) in actual clinical
practice(19). Even with stringent glycemic control
attained through the use of metformin and
sulfonylureas, patients with T2DM remain at a
significant risk of cardiovascular mortality and
renal failure. As per the 2018 guidelines provided
by the American Diabetes Association (ADA) and the
European Association for the study of Diabetes
(EASD), it is recommended to consider
cardiovascular risk or presence of chronic kidney
disease, following the initial treatment with
metformin. Additionally, patients with heart
failure or chronic kidney disease are advised to
use DPP-4i and SGLT2i(12). Recent clinical trial
data have also highlighted the better tolerability
profiles, minimal risk of hypoglycaemia and
convenient once-daily dosing, making them
particularly suitable for elderly diabetic
patients(20). However, there remains
underutilisation of this medication class,
potentially due to mixed data from clinical trials
regarding their safety profile(7).
One of the main
strengths of our study is the analysis of the
prescribing profile of SGLT2i, DPP-4i and
traditional antidiabetic agents across patients
based on their HbA1c values. The findings were
consistent across all HbA1c sub-cohorts, with the
highest risk identified in patients with HbA1c
levels between 7.5% and 9%. This subgroup
exhibited the highest prevalence of
diabetes-related complications, indicating a more
advanced stage of diabetes compared to other
subgroups. These findings align with a study by
Elvira D’Andrea et al., which also
reported similar results in diabetic patients with
HbA1c levels ranging from 7.5% to 9%(21).
The ADA-EASD (2018)
guidelines recommend the step-wise addition of
antidiabetic agents based on the patient’s HbA1c
values(11). Our study revealed that SGLT2i and
DPP-4i were often prescribed as triple or
quadruple therapy alongside metformin,
sulfonylureas and insulin for patients with HbA1c
levels above 8%. Most meta-analyses showed that
monotherapy with SGLT2i improves HbA1c levels by
0.5-1.0%. In our study, only 3% and 5.3% of
patients were initiated with SGLT2i and DPP-4i
respectively as monotherapy. Additionally,
combination therapy with SGLT2i or DPP-4i can
provide optimal efficacy for patients receiving
metformin without increasing the risk of side
effects(8,22). However, there is significant
geographical differences in the prescribing trend
of antidiabetic medications. For instance, the
Asian-HF registry, which recruited Asian diabetic
patients, reported that half of the patients were
on monotherapy and 37% on dual therapy(17). Our
study had 31.5% receiving monotherapy and 10.7% on
dual therapy.
The observed
contrast in the rate of prescribing of SGLT2i and
DPP-4i may be attributed to several factors.
Firstly, restricted access to these medications in
our settings might have led prescribers to reserve
them for patients at high risk of complications.
Secondly, the high cost of treatment may not be
affordable for all patients. Lastly, the
significant risk of genitourinary infections
associated with SGLT2i, particularly in women,
might have influenced prescribing decisions.
The variables that
were associated with the utilisation of DPP-4i and
SGLT2i in our study were patients with co-existing
CVD or CKD, patients aged > 65 years and male
patients with poorer glycaemic control, as well as
those who had more frequent visits from
nephrologist and cardiologist. Limited clinical
experience, knowledge and competency gaps among
providers may contribute to the restricted
prescribing of these newer agents(19,23,24). In a
similar study, disparities in SGLT2i prescribing
were noted, with markers of poorer glycaemic
control and male patients being linked to higher
odds of SGLT2i prescribing. Conversely, female
sex, advancing age and socioeconomic disparities
were linked to lower odds of being prescribed the
medication(25).
Our study reflected
the real-world prescribing pattern compared to the
highly selected population in clinical trials
which is the strength of the study. Also, the
prescribing trend of the antidiabetic agents was
stratified based on their HbA1c values. The study
had certain limitations. Since data were gathered
from a single hospital, the population was
relatively homogeneous. Therefore, the findings
may not apply to the general population. Secondly,
alpha glucosidase inhibitors (voglibose), GLP1-RAs
(exenatide) and glitazones (pioglitazone) were
excluded as their usage in the hospital was very
low. Thirdly, in our study, only 16.9% exhibited
uncontrolled blood sugar levels, potentially
explaining the under-prescription of the newer
agents.
Conclusion
The current study
highlights the prescription pattern of newer
versus traditional antidiabetic medications among
patients with T2DM and complications. There is
significant variation in prescription patterns
based on age, gender and prescriber speciality.
Traditional agents remain the most commonly
prescribed, whereas newer antidiabetics see low
prescription rates despite their benefits for T2DM
patients with complications. Efforts are needed to
identify the barriers to the utilisation of SGLT2i
and DPP-4i among this patient population.
Acknowledgement
We thank Dr Sudha
Bhanu, Medical superintendent at Karuna Medical
College and Hospital, Palakkad, Kerala, India for
her guidance and continuing support. We also thank
the Institutional Human Ethics Committee of Karuna
Medical College for timely approval of the
research proposal.
Conflicts Of Interest:
The author(s) do not have any conflict of
interest.
Ethics statement
Ethical clearance
was granted from the Institutional Human Ethics
Committee of Karuna Medical College and Hospital,
Palakkad, Kerala, under the study reference number
KMC/IHEC/15/2023.
Funding
Self-funded.
Informed consent statement
Written consent was obtained from all the
participants using an approved and locally
translated consent form. Patients were informed
about the details of the study, purpose, also
confidentiality was maintained through all stages.
References
- Thacker T. India tops global diabetes list
with 212 million cases in 2022: Lancet Study. The
Economics Times. 2024 Nov 13;
- Maiti S, Akhtar S, Upadhyay AK, Mohanty SK.
Socioeconomic inequality in awareness, treatment
and control of diabetes among adults in India:
Evidence from National Family Health Survey of
India (NFHS), 2019–2021. Sci Rep. 2023
Dec 1;13(1).
- Anjana RM, Unnikrishnan R, Deepa M et al.
Metabolic non-communicable disease health report
of India: the ICMR-INDIAB national
cross-sectional study (ICMR-INDIAB-17). Lancet
Diabetes Endocrinol. 2023 Jul
1;11(7):474–89.
- Arnouts P, Bolignano D, Nistor I et al.
Glucose-lowering drugs in patients with chronic
kidney disease: A narrative review on
pharmacokinetic properties. Vol. 29, Nephrology
Dialysis Transplantation. Oxford University
Press; 2014. p. 1284–300.
- Vora H, Kaur P. Prediabetes and diabetes in
India: An HbA1c based epidemiology study. Diabetes
Research and Clinical Practice.2024;217:111889
- Anjana RM, Unnikrishnan R, Deepa M et al.
Achievement of guideline recommended diabetes
treatment targets and health habits in people
with self-reported diabetes in India
(ICMR-INDIAB-13): a national cross-sectional
study. Lancet Diabetes Endocrinol. 2022
Jun 1;10(6):430–41.
- Narasaki Y, Kovesdy CP, You AS et al. Safety
of SGLT2 inhibitors, DPP-4 inhibitors, and GLP-1
receptor agonists in US veterans with and
without chronic kidney disease: a
population-based study. The Lancet Regional
Health - Americas. 2024 Aug 1;36.
- Ajmal M, Akhter S, Khushtar M. An Update On
Fixed-Dose Combination Of Sglt-2 And Dpp-4
Inhibitors In The Management Of Type-2 Diabetes
Section A-Research paper Eur. Available from:
https://www.researchgate.net/publication/372892117
- Chadha M, Das AK, Deb P et al. Expert Opinion:
Optimum Clinical Approach to Combination-Use of
SGLT2i + DPP4i in the Indian Diabetes Setting.
Diabetes Therapy. 2022 May
1;13(5):1097–114.
- Consensus on the use of DPP4 Inhibitors and
SGLT2 Inhibitors in T2DM with Chronic Kidney
Disease-from Indian Context. Diabetes Obes
Int J. 2021;6(2):1–14.
- Das AK, Gandhi P, Saboo B et al. Optimizing
the treatment of newly diagnosed type 2 diabetes
mellitus with combination of dipeptidyl
peptidase-4 inhibitors and metformin. J
Family Med Prim Care. 2021
Dec;10(12):4398–409.
- Suto G, Molnár GA, Rokszin G et al. Risk of
morbidity and mortality in patients with type 2
diabetes treated with sodium-glucose
cotransporter-2 inhibitor and/or dipeptidyl
peptidase-4 inhibitor: A nationwide study. BMJ
Open Diabetes Res Care. 2021 Jan 20;9(1).
- Mengdi Li. Efficacy and Safety of Triple
Therapy with SGLT-2 Inhibitor, DPP-4 Inhibitor,
and Metformin in Type 2 Diabetes: A
Meta-Analysis. ALTERNATIVE THERAPIES. 2023
Jul;29(5):320–6.
- Liaw J, Harhay M, Setoguchi S, Gerhard T, Dave
CV. Trends in Prescribing Preferences for
Antidiabetic Medications Among Patients With
Type 2 Diabetes in the U.K. With and Without
Chronic Kidney Disease, 2006–2020. Diabetes
Care. 2022 Oct 1;45(10):2316–25.
- Chang HY, Su YW, Feng AN et al. Prescription
patterns of diabetes medications influencing
clinical outcomes of heart failure patients with
reduced ejection fraction. ESC Heart Fail.
2020 Apr 1;7(2):604–15.
- Mahtta D, Ramsey DJ, Lee MT et al. Utilization
Rates of SGLT2 Inhibitors and GLP-1 Receptor
Agonists and Their Facility-Level Variation
Among Patients With Atherosclerotic
Cardiovascular Disease and Type 2 Diabetes:
Insights From the Department of Veterans
Affairs. Diabetes Care. 2022 Feb
1;45(2):372–80.
- Chia YMF, Teng THK, Tay WT et al. Prescription
patterns of anti-diabetic medications and
clinical outcomes in Asian patients with heart
failure and diabetes mellitus. European
Journal of Heart Failure. 2019;21:685–8.
- McMurray JJV, DeMets DL, Inzucchi SE et al.
The Dapagliflozin And Prevention of
Adverse-outcomes in Heart Failure (DAPA-HF)
trial: baseline characteristics. Eur J Heart
Fail. 2019 Nov 1;21(11):1402–11.
- Rhee JJ, Han J, Montez-Rath ME et al.
Antidiabetic medication use in patients with
type 2 diabetes and chronic kidney disease. J
Diabetes Complications. 2019 Nov 1;33(11).
- Du YF, Ou HY, Beverly EA, Chiu CJ. Achieving
glycemic control in elderly patients with type 2
diabetes: A critical comparison of current
options. Vol. 9, Clinical Interventions in
Aging. Dove Medical Press Ltd.; 2014. p.
1963–80.
- D’Andrea E, Wexler DJ, Kim SC, Paik JM, Alt E,
Patorno E. Comparing Effectiveness and Safety of
SGLT2 Inhibitors vs DPP-4 Inhibitors in Patients
with Type 2 Diabetes and Varying Baseline
HbA1cLevels. JAMA Intern Med. 2023 Mar
6;183(3):242–54.
- Sim R, Chong CW, Loganadan NK, Adam NL,
Hussein Z, Lee SWH. Factors associated with
DPP4i or SGLT2i utilisation: a retrospective
cohort study among people with type 2 diabetes
mellitus. Journal of Pharmacy Practice and
Research. 2024;
- Harris ST, Patorno E, Zhuo M, Kim SC, Paik JM.
Prescribing Trends of Antidiabetes Medications
in Patients With Type 2 Diabetes and Diabetic
Kidney Disease: A Cohort Study. Diabetes
Care. 2021 Oct 1;44(10):2293–301.
- Pantalone KM, Misra-Hebert AD, Hobbs TM et al.
Antidiabetic treatment patterns and specialty
care utilization among patients with type 2
diabetes and cardiovascular disease. Cardiovasc
Diabetol. 2018 Apr 10;17(1).
- Ozaki AF, Ko DT, Chong A et al. Prescribing
patterns and factors associated with
sodium–glucose cotransporter-2 inhibitor
prescribing in patients with diabetes mellitus
and atherosclerotic cardiovascular disease. CMAJ
Open. 2023 May;11(3):E494–503.
|



















